 Q: I have a 36-year-old female patient who’s been getting headaches
recently. Her vision is fine and she has no other complaints. However, she has
bilateral swollen optic discs. It appears to be papilledema, so I’m referring
her to a neurologist for further evaluation. What’s going on with this patient?
Q: I have a 36-year-old female patient who’s been getting headaches
recently. Her vision is fine and she has no other complaints. However, she has
bilateral swollen optic discs. It appears to be papilledema, so I’m referring
her to a neurologist for further evaluation. What’s going on with this patient?
A: “If it’s papilledema, you have to check for a brain tumor,” says neurologist Mark Kozinn, M.D., of Atlanta. “But in all my years of practice, I’ve yet to see my first brain tumor with papilledema. More than likely, this young woman has idiopathic pseudotumor cerebri.”
Indeed, this patient was referred to Dr. Kozinn, and his working diagnosis was pseudotumor cerebri—although he had to rule out the other possibilities of brain tumor and venous sinus thrombosis. In his evaluation, Dr. Kozinn performed a CT scan and a lumbar puncture. The scan was normal and the lumbar puncture showed elevated intracranial pressure.
“I placed her on acetazolamide, which is standard therapy for pseudotumor cerebri, and asked her to come back and see me within a couple of weeks,” Dr. Kozinn says. Pseudotumor cerebri typically occurs in heavyweight females of childbearing age. Classic symptoms include headache, blurred and/or double vision, a “whooshing” sound in the ears, vision loss, and pain with eye movement.
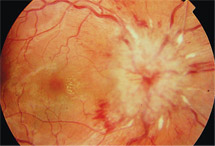 |
| This patient had bilateral disc swelling.
|
“She wasn’t just taking a lot of vitamins,” Dr. Kozinn says. “She was taking a ton of vitamins.” When asked, the patient explained she took many different vitamins—vitamins for her hair, her fingernails, her teeth, her eyes, as well as a daily multivitamin. She brought in all her vitamin bottles, and the nephrologist added up her daily intake of vitamin D as an example.
“He said, she’s poisoning herself with vitamin D,” Dr. Kozinn says. “I said, I bet she’s poisoning herself with vitamin A, too.” The recommended daily allowance of vitamin A for an adult woman is between 2,000 and 3,000 units. This patient was taking a cumulative dose of more than 7,500 units. Research indicates that excess vitamin A is linked to intracranial hypertension and papilledema.1,2
But it’s not clear how hypervitaminosis causes these changes. For comparison, “Several cases of pseudotumor cerebri have been documented in the literature in young patients being treated with retinoic acid for acute promyelocytic leukemia,” says Kimberly Reed, O.D., associate professor of ocular disease and therapeutics at Nova Southeastern College of Optometry. Retinoic acid is the acid form of vitamin A. “The mechanism for PTC in these patients is unclear, but it is possible that excessive retinoic acid interferes with the reabsorption of cerebral spinal fluid through the arachnoid villi.”3
In these patients, and in the young woman in this case, discontinuation of the vitamin A resolved the pseudotumor cerebri. Dr. Kozinn says he learned his lesson to always specifically ask about vitamin intake in cases of papilledema.
“Take a careful history of medications. Even something as benign as over-the-counter vitamins can result in an adverse consequence,” he says. “The patient thought she was doing something healthy. But sometimes too much of a good thing is just too much.”
1. Marcus DF, Turgeon P, Aaberg TM, et al. Optic disk findings in hypervitaminosis A. Ann Ophthalmol. 1985 Jul;17(7):397-402.
2. Lombaert A, Carton H. Benign intracranial hypertension due to A-hypervitaminosis in adults and adolescents. Eur Neurol. 1976;14(5):340-50.
3. Sano F, Tsuji K, Kunika N, et al. Pseudotumor cerebri in a patient with acute promyelocytic leukemia during treatment with all-trans retinoic acid. Intern Med. 1998 Jun;37(6):546-9.

