24th Annual Surgery ReportFollow the links below to read other articles from annual update on surgery: The Preoperative Ocular Surface Checkup Corneal Compromise: How to Assess the Risk of Post-LASIK Ectasia Excise and Conquer: Adding Minor Surgical Procedures to the Optometric Office |
No FDA-approved IOL provides true accommodation akin to that of the human eye, and with all pseudoaccomodating IOLs, increasing depth of field is associated with dysphotopsias in night vision. While some doctors avoid recommending presbyopia-correcting lenses altogether because of concerns related to possible dysphotopsias, it is important to consider that not correcting presbyopia surgically and relying on multifocal spectacles can have its own set of risks that are more than just an annoyance.
Multifocal (bifocal, trifocal and progressive) spectacles contribute significantly to the risk of trips and falls in the elderly. One study found that multifocal spectacle wearers were more than twice as likely to fall and that multifocal glasses accounted for nearly 41% of the attributable risk for falls outside the home.1 The Centers for Disease Control (CDC) reports that falls are a leading cause of injury and death in older Americans. In fact, an older adult falls every second of every day, leading to seven million injuries, and over 27,000 elderly deaths (more than from breast cancer or prostate cancer) annually.2 Falls also threaten the independence and quality of life of seniors.
Patients who fall do not typically go to their eye doctors; therefore, the eye care community has not appreciated the impact of these incidents on our patients. Nevertheless, since falls can be prevented, we should rethink our approach to treating presbyopia. We should at least consider prescribing separate glasses for distance and near, and we should also consider offering surgical options that reduce the need for progressive/multifocal glasses.
Fortunately, there are many good options to increase the depth of field surgically. Both referring optometrists and surgeons who may have been unhappy with the results of earlier technology should consider newer presbyopia-correcting IOL options, since they offer more advantages and fewer disadvantages compared to older designs.
 |
| Fig. 1. Ideally, with contrast and brightness both at 100%, there is no blur, providing a nice, sharp optotype and a high-quality visual experience. |
Approaches to Presbyopia Correction
Multifocal intraocular lenses, like multifocal contact lenses, split the focus of incoming light to increase depth of field, resulting in visual quality tradeoffs. The first multifocal IOLs used zonal refractive technology (more akin to the design of multifocal contact lenses) to split the light to far and near foci. Subsequent lenses used diffractive IOL technology to improve depth of field while improving visual quality both in the far and near (14” to 20”) ranges.
The first extended-depth-of-focus (EDOF) lens, the Tecnis Symfony (Johnson & Johnson Vision) also uses diffractive technology but includes an echelette design to correct the chromatic aberration present in the cornea for improved contrast sensitivity and to produce a pattern of light diffraction that elongates the focus. This extends the range of quality vision with a reduced amount of night vision symptoms. It also moves the region of functional near vision towards intermediate, so proper patient selection and education become important factors in the ultimate success of implantation.
 |
|
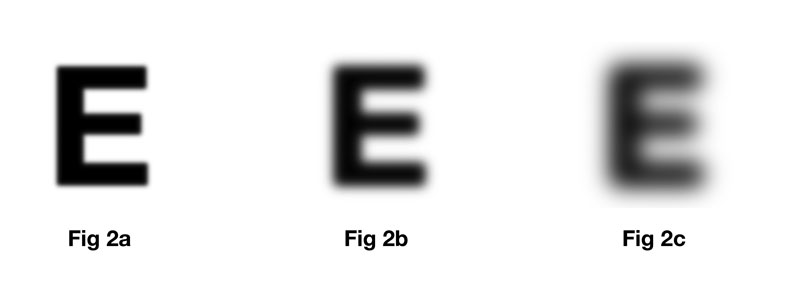
Fig. 2a-c. Increase in the transition between foreground and background causes blur as the relative sharpness at the edge decreases, making it increasingly difficult to distinguish a crisp separation. |
Optics and Visual Quality
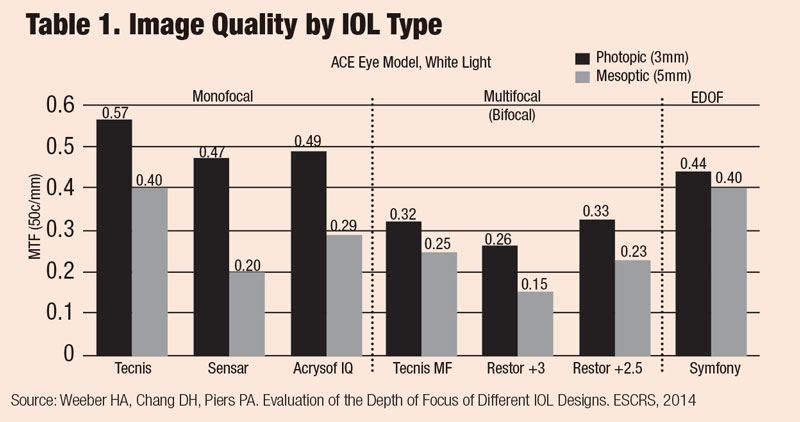
The visual quality or sharpness of vision is largely determined by the presence of optical aberrations, which are affected by the material, design and manufacturing of the implanted IOL. Although we often talk about monofocal IOLs as the standard for quality, there is a notable range of image quality even among monofocal lenses (Table 1). In particular, aspheric optics have been a major factor in improving visual quality in recent years. Addressing chromatic aberration with low dispersion (high Abbe number) materials can build upon this to continue improving image quality. The range of chromatic aberration among common IOL materials is comparable to the difference between crown glass and polycarbonate.
Patients rarely complain about visual quality after cataract surgery with monofocal IOLs. However, in those who opt for presbyopia correction too, there can be concerns about quality of vision. This can happen for several reasons: first, this latter group of patients tend to be younger and demand more from their vision; second, they are expecting to function well in many activities without glasses; third, they have invested out-of-pocket money to achieve these goals; and fourth, presbyopia-correcting IOLs do make optical trade-offs to increase depth of focus, and some IOL models even induce spherical and chromatic aberrations.
The Tecnis Symfony IOL, by correcting and minimizing chromatic aberration in addition to spherical aberration, demonstrates visual quality comparable to some monofocal IOL experiences. Petrotti et al. found no significant difference in contrast acuity or visual quality between the Tecnis Symfony and Tecnis monofocal IOLs, while patients with Symfony in fact had better uncorrected distance acuity and much lower dependence on glasses.3
 |
Postoperative Vision Complaints
In evaluating patients who have postoperative visual complaints despite objectively good visual acuity, it is helpful to group their concerns into one of two broad categories: daytime visual quality and nighttime dysphotopsias. While the optical etiologies of these visual side effects are related, they manifest in different ways clinically.
Both daytime visual quality and nighttime dysphotopsias are related to the visual effects of light from a visual target that is not focused optimally on the macula. When light from a particular point source is not in focus, whether from being defocused or scattered, it lies off the visual axis. A small amount of defocus of a large amount of energy or a large degree of defocus of a small amount of energy are the optical causes, respectively, of visual quality and dysphotopsia complaints.
 |
Fig. 3. Even a blurry image can be improved by magnification. Note that contrast is not reduced. |
Understanding Visual Quality
If patients have difficulties with daytime visual quality, they could be experiencing problems in one of two ways: blur and loss of contrast sensitivity. The difference can be illustrated by looking at the edges of optotypes on an eye chart.
When visual quality is good, an object or optotype has a clear transition from foreground to background, making it easy to identify and distinguish (Figure 1). As blur (or the spreading out of the transition between foreground and background) increases, the relative sharpness at the edge decreases, making it increasingly difficult to distinguish a crisp separation between foreground and background (Figures 2a-c). However, with a given amount of blur, magnifying the object (e.g., by moving it closer) can makes it easier to distinguish (Figures 3a-c).
Similarly, contrast (the difference in intensity between the background and the foreground) and brightness (light) help us to discern an object or optotype. In an ideal situation, contrast and brightness are both at 100%, and there is no blur, providing a nice, sharp optotype and a high-quality visual experience (Figure 1). However, with lower contrast (Figure 4a), decreased lighting (Figure 4b) or both (Figure 4c) the optotype becomes more difficult to see. For this reason, increased light can improve quality of vision in low contrast situations.
 |
Fig. 4a-c. Here, the images remain sharp (i.e., no blur) but Image resolution is reduced by lower contrast (4a), decreased lighting (4b) or both (4c). |
While it is paramount for the surgeon to correct refractive error and to select IOLs with excellent optical qualities, some postoperative visual problems can be addressed by the optometrist. Post-op refractive error continues to be the most common cause of visual complaints. A careful refraction can determine if glasses, or perhaps laser vision correction, may be helpful. When refracting an EDOF lens like the Tecnis Symfony, be sure to push plus (like for a young accommodating patient); the increased depth of field can cause autorefractors to overminus by up to 1.5D. Additionally, identifying treatable medical conditions like dry eye, posterior capsular opacification (PCO) or cystoid macular edema are important.
Less commonly, after implantation of a multifocal or EDOF lens, a patient might note that letters or objects are sharp but additionally note a “fuzziness, shadow, or glow” around them (Figure 5). Since there is a high-contrast sharp edge present, patients with these symptoms typically can still achieve good visual acuity and visual function. While there is no quick-fix for this symptom, patients typically just need reassurance and adequate time for neuroadaptation. Uncommonly, some patients may not be able (or willing) to adapt, and thus might be candidates for IOL exchange.
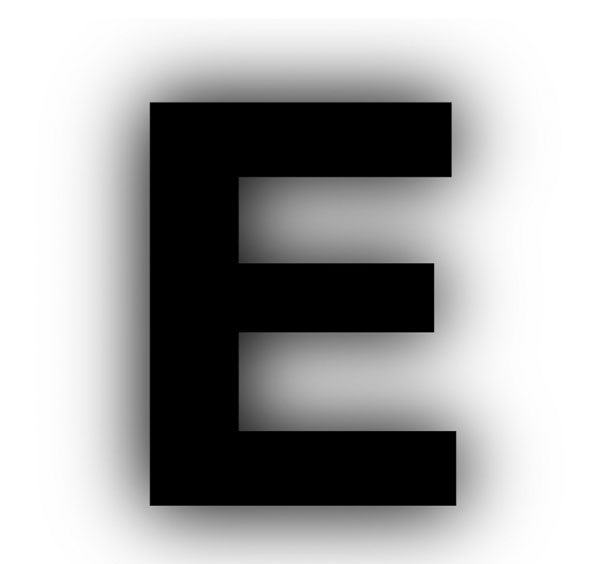 |
Fig. 5. A multifocal or EDOF patient may complain of “fuzziness” around objects. Contrast remains high, however, so explain the process of neuroadaptation. |
Dealing with Dysphotopsia
In addition to concerns about daytime visual quality, increasing the depth of field can also lead to dysphotopsias in low-light conditions, typically resulting in symptoms with night vision. Early-generation multifocal IOLs were associated with significant halos, but subsequent improvements in recent years have reduced some of these effects. Keep in mind that even some patients implanted with monofocal IOLs complain of night vision symptoms. Indeed, dysphotopsias are the primary source of patient dissatisfaction with all IOLs.
These visual symptoms, which vary widely in etiology and appearance, are the result of defocused and scattered light hitting the retina. Although they frequently occur in combination, for clinical trials the FDA classifies dysphotopsias into three distinct categories: glare/flare, halos and starbursts. Each has a different appearance to the patient and can occur for different optical reasons (Figure 6).
Glare or flare, which is a smearing or blur around a point source of light, can be due to refractive error, ocular surface problems, PCO and nuclear cataracts. It is less likely to be directly associated with any particular IOL optics.
Halos, which are one or more rings around a point source of light, are commonly associated with multifocal IOLs. These lenses have two distinct focal points with a dip in energy in between. Since the halo consists of the out-of-focus energy directed at the near focal point, the size of the halo is related to add power, with larger halos associated with higher add powers.
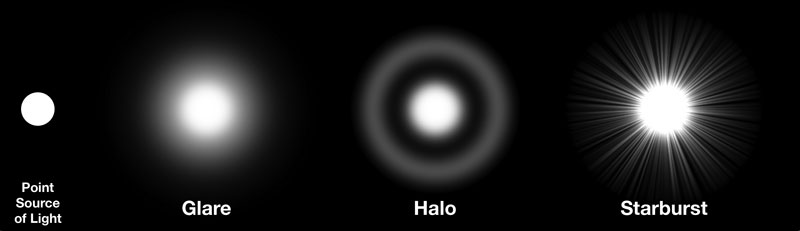 |
Fig. 6. Ask patients for as much detail as possible about any visual anomalies, and strive to use the same terminology. The above image depicts the three FDA categories of dysphotopia. |
Starbursts may be described by patients as streaks or rays of light emanating from a point source. These can occur with refractive error (especially astigmatism), ocular surface problems, posterior capsular folds, PCO or use of diffractive IOLs.
Newer presbyopia-correcting IOL designs provide new options, and trade-offs, between depth of focus and dysphotopsias. For example, while patients with diffractive multifocal IOLs tend to notice a single bright halo, patients with diffractive EDOF IOLs tend to describe starbursts and multiple fine concentric halos in a “spiderweb” pattern (Figure 7). In our practice, we have seen reduced night vision complaints with EDOF IOLs compared to multifocal IOLs, and appropriate preoperative counseling plays a critical role in how patients perceive their symptoms after surgery.
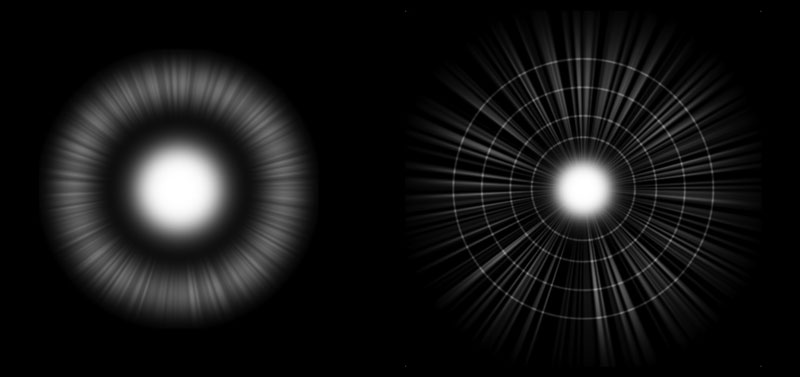 |
Fig. 7. Multifocal IOL patients may experience a single bright halo while those with diffractive EDOF IOLs tend to describe starbursts and fine concentric halos in a “spiderweb” pattern. |
Patient Counseling
When working to alleviate postoperative visual complaints, an ounce of prevention is worth a pound of cure. Preparing patients and setting expectations before surgery is key. Patients should be counseled that there will likely be some night vision symptoms but that they are usually tolerable.
For surgeons, it is no longer adequate simply to perform a procedure well. The ability to communicate the potential tradeoffs, to screen appropriate patients and to set proper expectations is crucial to the successful management of postoperative vision complaints.
If patients have visual complaints in the early postoperative period, it is important to diagnose the cause and to help the patient with appropriate behavioral and treatment approaches, whether that be providing more light, offering occasional reading glasses, considering refractive correction (spectacle or surgical), or treating medical conditions such as dry eye, PCO or CME.
Here, the optometrist is beginning to play an important role. Reassure patients that symptoms typically improve with time, healing and neuroadaptation for those able to do so. Referring optometrists should communicate with the surgeon if there is a significant or ongoing concern and refer back for further diagnosis and/or treatment, including lens exchange in the most refractory cases.
In conclusion, most well-chosen and fully prepped patients find the tradeoffs with modern presbyopia-correcting IOLs worthwhile and welcome the opportunity even if the initial results do not fully address every visual need. Concerns about visual quality and night vision problems, while not zero, are generally quite tolerable; and when patients are counseled appropriately before and after surgery, we maximize the chance of satisfaction with their visual outcomes.
Drs. Huggins and Chang are in practice at Empire Eye & Laser Center in Bakersfield, Calif. Dr. Chang is a consultant for Johnson & Johnson Vision.
1. Lord SR. Multifocal glasses impair edge-contrast sensitivity and depth perception and increase the risk of falls in older people. J Am Geriatr Soc 2002; 50:1760-6. 2. Centers for Disease Control. www.cdc.gov/media/releases/2016/p0922-older-adult-falls.html (Accessed 5/31/18) 3. Pedrotti E, Bruni E, Bonacci E, et al. Comparative analysis of the clinical outcomes with a monofocal and an extended range of vision intraocular lens. J Refract Surg 2016;32:436-42. |

