By Edward S. Bennett O.D., M.S.Ed. T
St. Louis, Mo.
The Role of the Laboratory
| Table 1: Resources the Laboratory Can Provide1 |
| 1. Experienced consultants to assist with contact lens design, fitting, troubleshooting and corneal topography analysis |
|
2. Fitting sets and inventories; loaner fitting sets are often available |
|
3. Specialty lens designs such as bifocal, bitoric and keratoconic lenses |
|
4. Resource materials such as fitting guides and videotapes |
|
5. Modification equipment and training |
|
6. Sponsorship of seminars and workshops |
The GP laboratory can provide a number of services to assist practitioners.1 Some of these resources are provided in Table One. Most important is the presence of trained consultants to assist you in material selection, lens design parameters and problem-solving for both spherical and specialty designs. This is especially important since approximately one-half of practitioners order GPs empirically, often providing keratometry values and the refraction to the laboratory, while 75% of practitioners simply indicate "standard" for their peripheral curve radii and widths.1,2
The most successful laboratories are those that provide the greatest number of services to practitioners and embrace new manufacturing technologies. The Contact Lens Manufacturers Association (CLMA) has a "Seal of Excellence" program, which rewards those laboratories who produce consistently high-quality lenses. With today"s high technology lathes, the machine that manufactures the lens can quickly and precisely make calculations that would take a human much longer, with less predictable results.
Lens Design
Overall Optical Zone Diameter (OAD/OZD). The first lens parameter to select is overall diameter. This will be dependent upon several factors but primarily on lid-to-cornea relationship and pupil size. Most lid-to-cornea relationships have at minimum a slight overlap of the lids over the limbus (see Figure 1). This relationship often results in the so-called "lid attachment" type of fit, in which the upper edge of the gas permeable lens positions under the upper lid. With patients exhibiting a larger-than-average palpebral aperture size where the upper lid is tangent to or above the limbus (see Figure 2), making a lid attachment fitting relationship very difficult to achieve, you"re best off using an interpalpebral fit. This necessitates a smaller-than-average overall diameter lens, which not only abuts the upper lid but will be positioned away from it; ideally it will be well centered on the cornea between the lids.
The overall diameter should be large enough to allow an optical zone diameter larger than the pupil size in dim illumination. Otherwise, the patient is likely to exhibit symptoms of flare under low illumination conditions, especially if the lens is decentered.
| Nine Essential Take-Home Points | |
| |
| |
| |
| |
| |
| |
| |
| |
|
Base Curve Radius (BCR). The base curve radius for any given patient depends upon several factors, including corneal curvature, lens power, lid-to-cornea relationship and fluorescein pattern evaluation. Because the cornea is aspheric and tends to flatten at a greater rate at an increasing distance from the center, selecting a base curve radius that is slightly flatter than "K" should result in an alignment fitting relationship. To optimize centration, use a steeper base curve radius with increasing corneal toricity; do likewise for plus lenses because of their more anterior center of gravity. A philosophy for base curve radius and diameter selection appears in Table 2.
Increasing the optical zone diameter of the lens will increase sagittal depth, effectively steepening the fitting relationship. Like-wise, reducing the optical zone diameter of the lens will decrease sagittal depth, effectively flattening the fitting relationship. A simple rule of thumb is to flatten the BCR by 0.25D for every increase in overall diameter of 0.5mm, and to steepen the BCR by 0.25D for every decrease in overall diameter of 0.5mm.3 The most common scenario is that in which you achieve an alignment fitting relationship with a patient exhibiting a large pupil size. A larger overall/optical zone diameter lens is indicated in this case; however, the base curve radius should be flattened by 0.25D at minimum to maintain the alignment fitting relationship.
 |
| FIG. 1: Normal lid-to-cornea relationship, which is optimum for lid attachment. (Courtesy of Ursula Lotzkat) |
 |
| FIG. 2: Large fissure size; strive for a small overall diameter, interpalpebral fitting relationship. (Courtesy of Craig Norman) |
Peripheral Curve Radii and Width. With today"s manufacturing technology, custom design of peripheral curves is becoming increasingly unnecessary. Aspheric or pseudo-aspheric peripheral curves are more popular and more reproducible, making GP lens design easier and more efficient. In fact, many of the newer standard designs use corneal topography to determine the periphery of a GP lens, which is often aspheric or pseudo-aspheric (i.e., several peripheral curves that are well blended). In addition, these designs are typically relatively low-edge clearance with little more edge clearance centrally than peripherally (see Figure 3). The lens parameter with the greatest impact on edge clearance is the outer peripheral curve radius and width.4,5 With PMMA lens designs, a flat, wide peripheral curve was used to optimize oxygen provided by tear circulation. However, the oxygen permeability of current GP lens materials negates the need for a high rate of tear exchange, whereas the potential drying effects of a high-edge clearance design are eliminated as well. It has been found that a high-edge clearance design funnels in surrounding tears, resulting in drying of the three and nine o"clock peripheral corneal regions, and it potentially affects blink quality through an increased interaction between the lens edge and the superior lid.6-11 When custom designing peripheral curves, at minimum, a tricurve or tetracurve design should be used with an outer curve that is no flatter than 11.00mm and no wider than 0.3mm. With young patients who participate in sports, using a larger-than-average overall diameter with a low-edge clearance lens design minimizes any risk of dislodgement and loss.
Using a well-blended peripheral curve system is also important. A poorly-blended or unblended peripheral curve system can produce dryness, itchiness, and scratchiness.12
| Table 2: GP Diameter and Base Curve Selection* | |||
| CORNEAL | OAD/OZD | ||
|
| |||
| Cylinder | 9.0/7.6mm | 9.4/8.0mm | 9.8/8.4mm |
| (interpalpebral & steep corneas) | (lid attachment) | (large pupils & athletes) | |
|
| |||
| 0 0.75D | 0.25D flatter than K | 0.50D flatter than K | 0.75D flatter than K |
|
| |||
| 1.00 1.25D | "On K" | 0.25D flatter than K | 0.50D flatter than K |
|
| |||
| 1.50 1.75D | 0.25D steeper than K | "On K" | 0.25D flatter than K |
|
| |||
| 2.00 2.25D | 0.50D steeper than K | 0.25D steeper than K | "On K" |
|
| |||
| >= 2.50D | A bitoric lens design is recommended | ||
|
| |||
| *For minus powers only; for plus powers, select a BCR 0.50D steeper than this philosophy | |||
Center Thickness. Center thickness is an important parameter for flexible GP lens materials. If the lens is too thin, flexure and instability can result. If the lens is too thick, its mass may result in inferior positioning on the cornea. The latter situation is especially problematic with GP lenses: studies show that increasing the center thickness by 0.04mm decreases the equivalent oxygen percentage (EOP) by less than 1% but will increase mass by 24%.13 Fortunately, advanced manufacturing techniques and instrumentation have led to the development of numerous ultrathin lens designs with center thicknesses up to 50% thinner than standard designs (for example, .10mm for a 3.00D lens as compared to a .15mm for a standard design).14,15 With the exception of high corneal astigmatism (> 1.50D), an ultrathin lens should be the design of choice in most spherical RGP lens fits. In high corneal astigmatism, a steeper than "K" base curve often results in flexure-induced reduction in visual acuity.16,17
| Table 3: Clinically Significant Parameter Changes20 | |
| Parameter |
Amount of Change for Clinical Significance |
|
| |
| Base Curve Radius |
0.50D (approx. 0.1mm) |
|
| |
| Overall Diameter |
0.4mm |
|
| |
| Optical Zone Diameter |
0.3mm |
|
| |
| Secondary Curve Radius |
0.3mm |
|
| |
| Peripheral Curve Radius |
0.5mm |
|
| |
| Center Thickness (for high Dk GPs) |
0.02mm |
Lenticular Applications. A lenticular design is sometimes indicated when the variance in edge thickness results in changes in lens power and overall diameter. In a lenticulated lens, the front surface consists of a central optical area surrounded by a peripheral carrier portion that is thinner and flatter. The junction of the optic cap and carrier section should have a thickness of 0.12-0.14mm.19,20 For lens powers of 5.00D or greater, I recommend a plus lenticular, since the edge thickness is typically 0.20mm or greater without this modification.21 A plus lenticular can minimize problems associated with thick edges, such as lens awareness, inferior positioning from lid-lens interaction and corneal desiccation resulting from compromise in the normal blinking process. A minus lenticular design is recommended with minus powers of 1.50D or less and all plus powers. It is used to increase edge thickness and therefore enhances lid interaction with the edge. It also minimizes inferior decentration. An edge thickness 0.06mm greater than the junction thickness is recommended.20
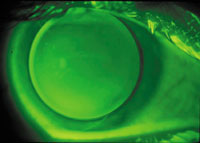 |
| FIG. 3: An alignment fitting relationship with slightly greater peripheral clearance. |
Another important consideration pertains to the effects of decentration. Inferior decentration increases the risk of corneal desiccation.23 As mentioned previously, the effect of reducing lens mass via an ultrathin lens design -- whenever possible -- should reduce the possibility of inferior decentration. Using a lenticular design as recommended also helps to optimize centration.
| Table 4: RGP Lens Institute GP Lens Design and Fitting Resources (available at www.rgpli.org) | |
|
Videotapes | |
|
1. |
GP Fitting and Evaluation: GP fluorescein pattern evaluation; base curve-diameter interaction; peripheral curve changes. |
| 2. | GP Problem-Solving Part One: Case Grand Rounds pertaining to myopic, hyperopic, high with-the-rule astigmatic, against-the-rule astigmatic, keratoconic and presbyopic patients; management of GP-induced problems such as adherence, desiccation, surface deposits, warpage and flexure. |
| 3. | GP Problem-Solving Part Two: Refitting of GP lenses; management of GP lens decentration. |
|
| |
| GP lens evaluation, fitting and problem-solving. | |
|
| |
| GP benefits, applications, fluorescein patterns and design/fitting pearls. | |
First and foremost, make the patient"s first experience with GP lenses a positive one. Diagnostic fitting of GP lenses traditionally has been the method of choice for numerous reasons. First, it allows patients to experience GP lens sensation and to leave the office having overcome the initial psychological hurdle of having lenses on their eyes. This often results in greater enthusiasm for lens wear on the patient"s part and greater confidence on the fitter"s part. Because you are competing with soft lenses, it is imperative that the patient"s initial experience is positive, both with comfort and -- if possible -- vision. This process begins with topical anesthetic use at the fitting visit to optimize initial comfort. This is followed by providing a lens from a large diagnostic fitting set or preferably from an inventory very close to the patient"s indicated power. If this is not possible, empirical fitting is recommended. Never underestimate the powerful effect on a new patient when you provide good vision after initial application of a GP lens. If the appropriate diagnostic lens power is not available via inventory or trial set, it makes sense to order a lens empirically to lessen the psychological effect of lens awareness.
The RGP Lens Institute (RGPLI) offers numerous educational resources to assist practitioners in designing, fitting, and troubleshooting spherical GP lenses (see Table 4). You can access them via the RGPLI website, www.rgpli.org.
The introduction of more reproducible ultrathin designs with standard peripheral curves has made GP lens design much easier. Likewise, if the initial patient experience is relatively comfortable, fitting GP lenses need not be any more challenging and time-consuming than fitting soft lenses.
Dr. Bennett is an associate professor of optometry at the University of Missouri, St. Louis College of Optometry, and is executive director of the RGP Lens Institute.
References
1. Bennett ES. Detailing your RGP Rx. Contact Lens Spect 1998;13(10).
2. Schwartz CA, Bennett ES, Moore C. Setting standards: what is a peripheral curve? Contact Lens Spect 1997;12(10).
3. Bennett ES. Lens design, fitting and evaluation. In Bennett ES, Henry VA: Clinical Manual of Contact Lenses (2nd ed.), Philadelphia: Lippincott Williams & Wilkins, 2000, pp. 75-124.
4. Caroline PJ, Norman CW. A blueprint for RGP design, Part 1. Contact Lens Spectrum 1988;3:39-49.
5. Bibby MM. Factors affecting peripheral curve design. Am J Optom & Physiol Opt 1979;56(1):2-9.
6. Bennett ES. The effect of varying axial edge lift on silicone/acrylate lens performance. Contact Lens J 1986;14:3-7.
7. Schnider CM, Terry RL, Holden BA. Effect of patient and lens performance characteristics on peripheral corneal desiccation. J Am Optom Assoc 1996;67(3):144-50.
8. Stone J. Designing hard lenses in the 1980s. J Br Contact Lens Assoc 1982;4(4):144-50.
9. Holden T, Bahr K, Koers D, Edrington T. The effect of secondary curve liftoff on peripheral corneal desiccation. Poster presented at the Annual Meeting of the American Academy of Optometry, Denver, Colorado, December 1987.
10. Bell GR. A new theory on 3 and 9 o"clock staining. Contact Lens Spect 1997;12(12).
11. Edwards K. Rigid gas-permeable contact lens problem solving. Optician 2000;219(5740):18-24.
12. Picciano S, Andrasko GJ. Which factors influence RGP lens comfort? Optom Today 1989;4(5):31-3.
13. Hill RM, Brezinski SD. The center thickness factor. Contact Lens Spect 1987;2(10):52-4.
14. Norman C. Today"s RGPs: better performance through innovative technology. Contact Lens Spect 1996;11(11).
15. Achiron LR. Custom-designed ultra-thin RGP lenses. Contact Lens Spect 2001;16(5).
16. Pole JJ, Kochanny L. The comparative flexure of Polycon II, Silcon and Boston II contact lenses on toric corneas. Optom Month 1984;75(4):151-55.
17. Corzine JC, Klein SA. Factors determining contact lens flexure. Optom Vis Sci 1997;74(8):639-45.
18. Edwards K. Rigid gas-permeable contact lens problem solving. Optician 2000;219(5740):18-24.
19. Bier N, Lowther GE. Lens design. In Bier N, Lowther GE: Contact Lens Correction. Stoneham MA: Butterworths, 1977.
20. Snyder C. Designing minus carrier RGP lenses. Contact Lens Spect 1998;13(12).
21. Lowther GE. Review of rigid contact lens design and effects of design on lens fit. Int Contact Lens Clin 1988;15(12):378-89.
22. Szczotka LB. RGP parameter changes: how much change is significant? Contact Lens Spect 2001;16(4).
23. Henry VA, Bennett ES, Forrest JF. Clinical investigation of the Paraperm EW rigid gas-permeable contact lens. Am J Optom Physiol Opt 1987;64:313-20.

