 |
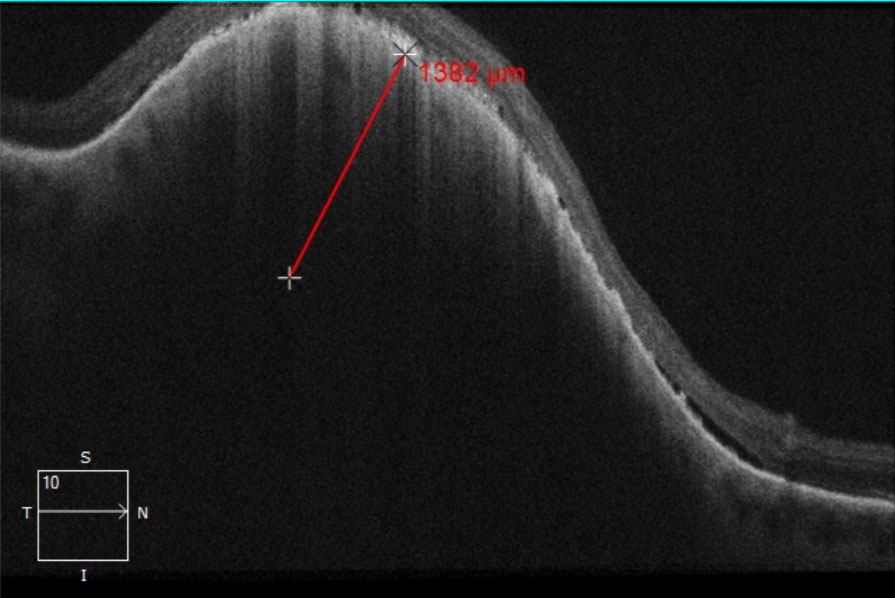
| Increased mortality risk of those receiving surgery-only therapy may be due to advanced stage at presentation rather than therapy selection, since Medicaid patients are likely presented with larger tumors compared with non-Medicaid patients. Photo: Amy Bade, OD. Click image to enlarge. |
With treatment paradigms in ocular cancers shifting away from complete enucleation, more research is needed on patient survival outcomes and potential socioeconomic disparity. The standard-of-care for small- to medium-sized uveal melanomas (UM) is radiation therapy; however, this is often only accessible at specialized centers that Medicaid patients may have limited access to.
To better elucidate the survival outcomes of patients with UMs based on Medicaid status, researchers collected information from the Surveillance, Epidemiology and End Results Medicaid database. This topic has not yet been discussed in literature, especially contextualizing the results, the researchers pointed out in their paper for Ophthalmic Epidemiology.
A total of 1,765 patients were included; of these, 95% were white and the average age was 52. There were no differences in five-year survival rates of those enrolled in Medicaid vs. those not, nor was Medicaid enrollment associated with increased mortality risk when compared with non-Medicaid enrollment in UM patients. However, Medicaid patients were found more likely to be unmarried, live in high poverty neighborhoods and live in rural areas. Increased risk of mortality was linked to factors of age and a tumor size greater than 10mm.
Expanding upon these findings, the study researchers explained that Medicaid enrollment before UM diagnosis and longer duration of enrollment were both not associated with increased mortality risk. This was unexpected, since Medicaid enrollment has been linked in multiple previous studies with worse outcomes spanning many different cancer types. What’s more, survival rates were 86.6% in the Medicaid group and 85.5% in the non-Medicaid group.
Worse cancer outcomes for those with Medicaid may be due to advanced tumor stage at time of clinical presentation. In this population, though, there was no difference in tumor size or tumor stage at time of presentation, a surprising outcome, because cancer outcome disparities are largely driven by more advanced stage at diagnosis. This is particularly notable because the Medicaid group was more likely to be from high- to medium-poverty where there is less likelihood of receiving early preventative screening.
Other than the factors of age and tumor size contributing to mortality rate, so did the administration of therapy with surgery. This echoes the findings of one previous study that reported mortality peak after receipt of enucleation, potentially from metastatic cells released after surgery. Medicaid patients were more likely to receive treatment involving surgery, but recent research also shows non-surgical form of ocular therapy like episcleral plaque radiation and proton beam radiation therapies to also show similar increased mortality. In this way, mortality peak for both surgical and non-surgical options may just reflect natural UM progression.
Overall, the authors relay that “the results from this study suggest that patients enrolled in Medicaid are not at higher risk of UM cancer-specific mortality due to poor screening (and thus presenting with more advanced staged cancer) nor due to more limited treatment options due to their insurance status.”
Despite the relatively positive outcomes, the team advised that “further investigation is needed to evaluate the impact of insurance and socioeconomic status on cancer outcomes in this patient population.”
Kim EJ, Lee JY, Ganga A, et al. Analysis of uveal melanoma 5-year survival rates by Medicaid status: a nationwide analysis. Ophthalmic Epidemiol. November 15, 2023. [Epub ahead of print]. |

