A 69-year-old white male presented for his annual eye exam. He had no new visual complaints, but he mentioned a longstanding floater in his right eye that had been diagnosed two years earlier as a posterior vitreous detachment.
His medical history was significant for hypertension, hyperlipidemia and depression. Medications included lisinopril, Lipitor (atorvastin calcium, Pfizer), Serzone (nefazodone, Bristol-Myers Squibb), and 81mg aspirin.
Diagnostic Data
Best-corrected acuity was 20/25 O.U. Pupils were equal, round, reactive to light, and there was no afferent pupillary defect. Extraocular muscles and adnexa were normal in both eyes. Slit lamp examination of the lids, conjunctivas, corneas, anterior chambers and irides were unremarkable. Grade 1 nuclear sclerosis was found O.U. IOP measured 17mm Hg in each eye.
The dilated fundus exam revealed a cup-to-disc ratio of 0.4 O.D. and 0.6 O.S. with temporal pallor O.U. Also, fine drusen was found in the maculae. A posterior vitreous detachment was observed in the right eye. The retinal periphery was flat and intact in both eyes.
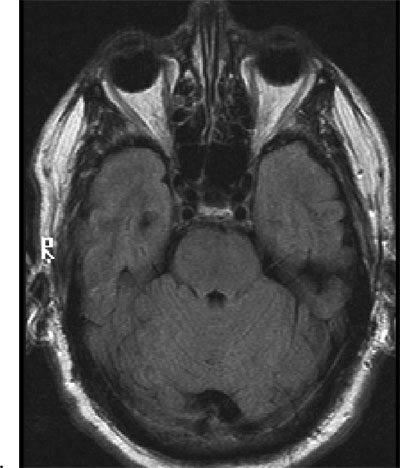
1. The initial fundus and optic nerve presentation O.D. (top) and O.S.
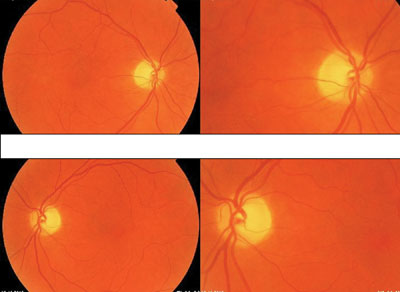
We reviewed the patients previous exam records. He had been examined two years earlier, at which time he had a cup-to-disc ratio of 0.4 O.U. Last year, the same observer again noted a 0.4 cup-to-disc ratio O.U. The patient was identified as a glaucoma suspect, and disc photos were taken (figure 1).
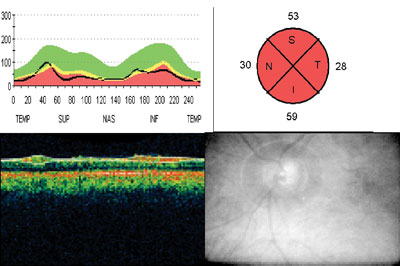
We ordered optical coherence tomography (OCT) due to the asymmetry and changes in the cup-to-disc ratio (figures 2 and 3). Thinning of the peripapillary retinal nerve fiber layer was found at the 1% (red) level in both eyes (53m O.D., 44m O.S.).
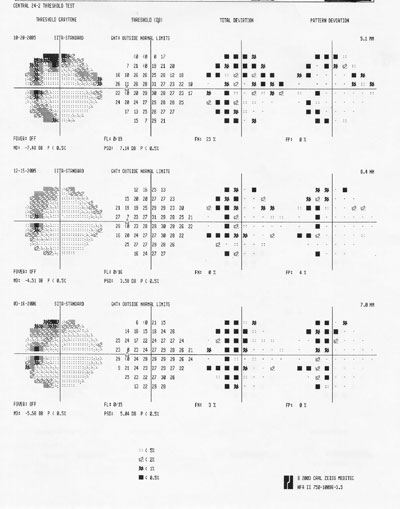
The patient returned for Humphrey 24-2 visual fields two months later. These showed superotemporal depressions O.D. and temporal depressions O.S. that were concentrated near the vertical midline in each eye (figures 4 and 5). The false negatives were 11% O.D. and 23% O.S. Repeat visual field testing yielded false negatives at 0% O.U., suggesting repeatable bitemporal hemianopsias. A 120-point visual field was then taken, which verified a bitemporal hemianopsia. The 24-2 visual fields were repeated two additional times over the next five months.
2. OCT right eye peripapillary retinal nerve fiber layer scan.
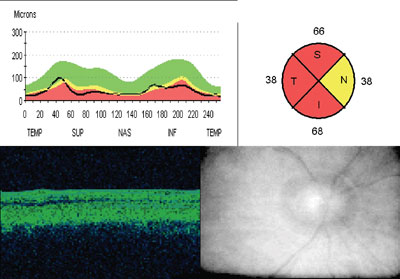
The pachymetry readings were 540m O.D. and 551m O.S. The OCT was repeated and found to be unchanged with a high signal strength and reliability. IOP was 16mm Hg O.D. and 15mm Hg O.S.
The patients recent lab work-upa complete blood count, glycosylated hemoglobin (A1C), lipids, and comprehensive metabolic panelwere unremarkable. A prolactin lab was ordered and was also normal. The patient reported experiencing elevated blood pressure and dizziness, and that he had been working with his primary care physician to gain better control.
3. OCT left eye peripapillary retinal nerve fiber layer scan.
The patient was sent that day for computed tomography (CT) scan of the head with and without contrast to rule out a pituitary adenoma. The radiologist diagnosed mild generalized cerebral atrophy consistent with age. There were no masses or aneurysmal formation. He recommended a magnetic resonance imaging/magnetic resonance angiograph (MRI/MRA) of the brain, which found no sign of compressive lesions or other explanation of the patients symptoms (figure 6). In particular, there were no signs of pituitary adenoma.
The patient was referred to ophthalmology for further evaluation. He demonstrated normal color vision and no peripheral neuropathies, except for an area of bilateral numbness on the lateral thigh attributed to L3-5 disc disease. The patient was sent back to optometry for continued observation without any identified cause of the field loss. After a review of all the previous testing, Vitamin B12 (Cobalamin) and folate labs were ordered in hopes of explaining the bitemporal visual field loss.
4. Right eye 24-2 Humphrey serial visual fields.

Diagnosis
The patients vitamin B12 (cobalamin) level was found to be low, at 175 pg/mL. Normal range is 240 pg/mL to 900 pg/mL.
Treatment and Follow-Up
We referred the patient to his primary-care provider for treatment and management. He began a one-month course of oral B12 vitamins, to be modified to injections if his levels remained low. But, at one month, his B12 level was 582 pg/mL, so he continues to be
monitored. His visual fields and peripapillary nerve fiber layer have remained stable.
Discussion
Visual field loss is often the initial manifestation of disorders involving the optic chiasm.1
Hemianopic defects and preferential involvement of the temporal visual field are the earliestand most commonvisual symptoms.1 There are multiple etiologies of chiasmal lesions, including congenital, traumatic, iatrogenic (secondary to radiation treatment), intrinsic (gliomas) and extrinsic lesions. Most chiasmal syndromes can be categorized as intrinsic (thickening of the chiasm itself) or extrinsic (compression of the chiasm from an adjacent structure).1 Extrinsic lesions are typically caused by pituitary tumors, craniopharyngiomas, and meningiomas, but they can also result from aneurysms and lesions of the sinuses.1
Vitamin B12 has a role in folic acid metabolism, so it is necessary for DNA synthesis, hematopoiesis, nerve growth, myelin synthesis and nervous system integrity. Vitamin B12 forms a complex with intrinsic factor before being absorbed from the ileum and stored in the liver.2 Inadequate dietary intake, malabsorption syndromes, hypermetabolic state, pregnancy, and megaloblastic anemia can also cause vitamin B12 deficiency.2 Normal absorption of the vitamin always exceeds body needs, so excess B12 is excreted in the urine.2
5. Left eye 24-2 Humphrey serial visual fields.
Vitamin B12 occurs naturally as the product of specialized microorganisms that grow in, or serve as food supply to, those animals below humans in the food chain.3 Nearly all dietary vitamin B12 comes from animal products.3
Documented cases of rare chiasmal lesions causing typical chiasmal visual field defects, such as bitemporal hemianopsia or junction scotoma, include demyelinating disease, vasculitis, and cobalamin deficiency.4 For example, one case involved a 29-year-old female with bitemporal hemianopsia, normal MRI scan, normal computed tomography (CT) scan, and normal visual evoked potential (VEP). She had only one-third of the normal amount of B12, but her blood counts were almost normal; only her hemoglobin value was decreased, and there was no sign of pernicious anemia. Vitamin B12 deficiency may exist without hematological manifestations. The cause of the vitamin B12 deficiency was not identified in this patient, and her intestinal update was normal.4
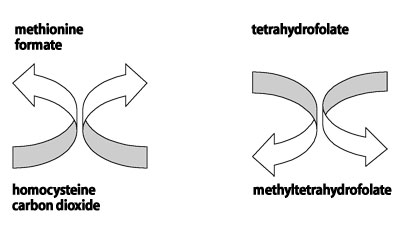
What is the mechanism in B12 that causes optic neuropathy? Vitamin B12, in the form of methylcobalamin, is required as a cofactor for the enzyme methionine synthetase, which then catalyzes the recycling of homocysteine to methionine (figure 7).5
So, a deficiency of vitamin B12 or folate could result in inadequate detoxification of endogenous formate and subsequent formic acidemia.5 Possibly, vitamin B12 optic neuropathy is a type of adenosine triphosphate (ATP) deficiency.6 Formate inhibits cytochrome C and results in decreased ATP production. Many people who use or consume tobacco and alcohol may have deficiencies of folate, vitamin B12 or both. However, only a small percentage will develop visual system dysfunction, and these patients may have a genetic predisposition for developing this type of optic neuropathy.5
6. Patients unremarkable MRI of the head and orbits.
An estimated 12% to 20% of community-dwelling North American elderly are cobalamin (B12) deficient.7 Cobalamin supplementation with a monthly intramuscular injection is the standard treatment for this condition. But, during the past 40 years, abundant evidence has been published indicating that high-dose oral cobalamin is as efficacious as the parenteral form.7
Vitamin B12 deficiency causes anemia, fatigue, loss of appetite, mood disturbances, paresthesias, ataxia, and memory loss.8 The process of vitamin B12 absorption can be impaired at the level of the stomach, where intrinsic factor is produced, or at the level of the terminal ileum, where intrinsic factor bound to vitamin B12 is absorbed.8 Medications, such as metformin or antacids, also can impair absorption.8 But, a small amount of vitamin B12 is absorbed by passive diffusion without intrinsic factor.8 Vitamin B12 is available over the counter in the form of tablets (100, 500, 1,000, or 5,000mg) and lozenges (50, 100, 250, or 500mg).8
7. The relationship between folate, vitamin B12 and formate.5
Vitamin B12 (cobalamin) deficiency should be considered in the differential diagnosis of any patient with optic nerve cupping, normal IOP and bitemporal visual field loss. Though the visual field loss is an uncommon finding, optometrists can more easily identify this subgroup of patients with vitamin B12 deficiencies than primary-care physicians. Risk factors for developing this deficiency include malnutrition, tobacco or alcohol abuse, age and any type of malabsorption disorder.
This patients only identified risk factor was age. He denied a history of tobacco or alcohol abuse or malabsorption syndrome, and reported that he ate a balanced diet.
Some patients may experience an improvement and partial recovery of visual function after vitamin B12 supplementation.4 Our patient was examined four months after starting vitamin B12 supplementation, and his visual field remained unchanged.
1. Foroozan R. Chiasmal syndromes. Curr Opin Ophthalmol 2003 Dec;14(6):325-31.
2. Tilkian S, Conover M, Tilkian A. Clinical & nursing implications of laboratory tests.
3. Widmann F. Clinical interpretation of laboratory tests.
4. Wilhelm H, Grodd W, Schiefer U, Zrenner E. Uncommon chiasmal lesions; demyelinating disease, vasculitis and cobalamin deficiency. Ger J Ophthalmol. 1993 Aug;2(4-5):234-40.
5. Golnik K, Schaible E. Folate-responsive optic neuropathy. 1994 Sep;14(3):163-9.
6. Rizz JF, Lessel S. Tobacco amblyopia. Am J Ophthalmol 1993;116:84-8.
7. Graham ID, Jette N, Tetroe J, Robinson N, Milne S, Mitchell SL. Oral Cobalamin remains medicines best kept secret. Arch Gerontol Geriatr. 2006 Apr 29; [Epub ahead of print].
8. Kripke C. Is oral Vitamin B12 as effective as intramuscular injection? Am Fam Physician. 2006 Jan1;73(1):65.

