Zoom in on Contact LensesThis August issue is our 46th annual contact lens report, where we help you use new and old techniques to improve your fitting skills. Check out the other featured articles here:
|
Comfort is a driving factor in patients’ contact lens success. It is well known among eyecare practitioners that most contact lens wearers experience contact lens discomfort at least occasionally, although many experience it to the degree that it alters their wearing habits and, in some cases, forces the patient to discontinue contact lens wear completely.1
Discomfort is the leading cause of contact lens discontinuation, also known as contact lens drop out.2 In fact, 36% of new contact lens wearers cite discomfort as their reason for dropout, second only to problems with vision (41%).3
A recent review of soft contact lens materials, designs and fitting characteristics found that surface properties affect the coefficient of friction of a lens and therefore play a large part in lens comfort.4 Surface treatments can include modifications of the lens material, addition of wetting agents or various structural changes at the outer surface of the lens.4
It is the search for comfort that continues to drive innovation and development of improvements in the contact lens space—whether it be the advancement of soft lens materials, addition of novel coatings for gas permeable lenses or the further customization of scleral lens design options—all aimed to improve the patient wearing experience.
Scleral lenses have made gas permeable (GP) lenses appetizing again, and as a result, there is a renewed focus on finding ways to perfect the process of making GP lenses. This is an exciting time for this vision-restoring modality and the industry has responded with ways to address the issues with lens fogging and poor wettability, as well as how to optimize patient comfort. However, to first understand the lens technology of today, we first must take a brief detour into the past.
 |
|
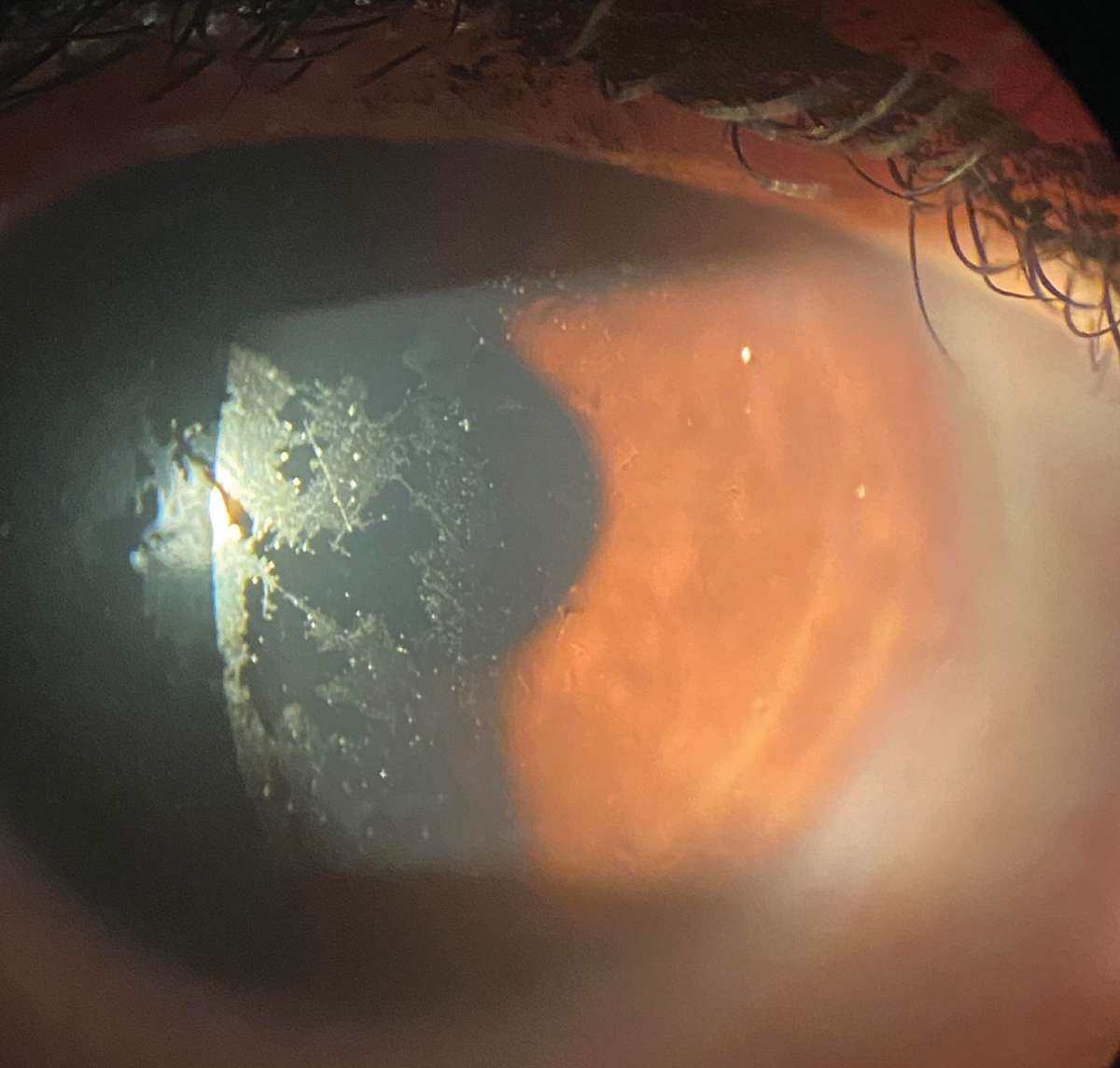
A patient complaining of discomfort and foggy vision, showing poor wettability of their scleral lens. The issues resolved with the addition of a Hydra-PEG coating. Click image to enlarge. |
GP Lens Material Evolution
Rigid lens manufacturing began with polymethylmethacrylate (PMMA) material. Its advantages included high durability, excellent optical quality, and ease of care; however, it was lacking in benefits to corneal health and physiology. PMMA had an oxygen transmissibility of (Dk) of zero, so practitioners had to ensure excellent tear exchange under the lens to achieve a healthy fit.5
The next evolution of lens material was the addition of silicone, which allowed more oxygen transmission through the lens instead of around it. These materials were referred to as silicone acrylates, and they’re still available today. The addition of silicone made the material hydrophobic and although the increased Dk was desirable, it came along with lens surface deposition, rapid drying of the tear film over the lens surface which resulted in dryness, as well as warpage, crazing and brittleness.6 However, silicone acrylates aren’t used as much because of poor wettability, surface deposits and patient discomfort.5
The next major step was adding fluorine to lens materials, which brings us to the widely used material in practice today: fluorosilicone acyrylate. Fluorine is known for its nonstick properties—such as in Teflon-coated cooking materials—increasing the deposit resistance of the lens materials.6 Adding fluorine lowered surface tension, decreased the attraction of polarized tear components to the lens surface and reduced the problem of ocular dryness. Comparison studies concluded that fluorosilicone acrylate lenses are more wettable and are perceived as more comfortable by patients than silicone acrylate lenses.7,8
Table 1. GP Materials to which Tangible Hydra-PEG Can Be Applied
| Material | Manufacturer |
| Boston ES | Bausch + Lomb |
| Boston EO | Bausch + Lomb |
| Boston XO | Bausch + Lomb |
| Boston XO2 | Contamac |
| Optimum Classic | Contamac |
| Optimum Comfort | Contamac |
| Optimum Extra | Contamac |
| Optimum Extreme | Contamac |
| Optimum Infinite | Contamac |
| HEXA100 | Contamac |
| HDS | Paragon |
| HDS100 | Paragon |
| FP-30 | Paragon |
| FP-92 | Paragon |
| Acuity 200 | Acuity Polymers |
Surface Treatments
Silicone-based materials are inherently hydrophobic, so any exposed silicone in a lens has the potential to be non-wetting. Additionally, some patients have excessive lipids in their tear film which may deposit onto the lens creating a foggy, hydrophobic surface. This issue can be reduced by dispensing low-silicone-content or hydrogel soft contact lenses; however, such lenses also impede oxygen transmission, increasing the chance for neovascularization, endothelial dysfunction or corneal edema.
Other solutions may include ensuring lid hygiene and treating the lens with plasma. However, non-wetting continues to plague both patient and practitioner alike, suggesting these options are insufficient.
There are two lens surface treatments available for contact lenses: plasma treatment and Tangible Hydra-PEG coating (Tangible Science), which is quickly becoming standard in high-end GP patient care.
 |
|
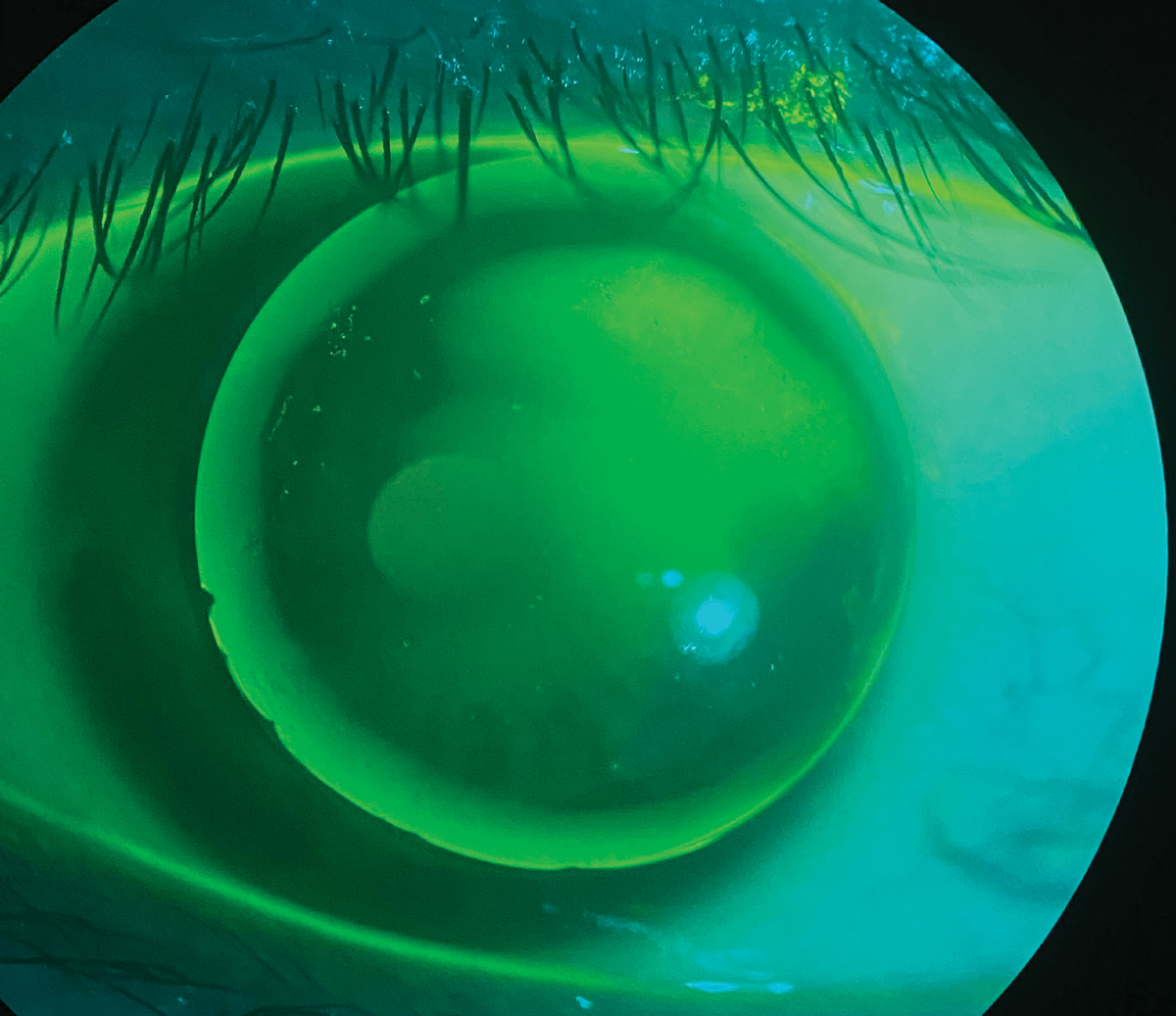
A patient wearing a GP lens presenting with issues of severe discomfort and peripheral corneal staining from a chipped edge. Click image to enlarge. |
Plasma. This is one of the most misunderstood elements in GP manufacturing. It is not an actual coating but a treatment or process wherein a newly manufactured lens is bombarded with high-energy radio waves in an oxygen-rich ionized gas chamber. The oxygen radicals strike the surface of the lens, dislodging hydrocarbons such as oils that may have been picked up in the manufacturing process.9 Nothing is being permanently added to the lens; rather, the process modifies the lens surface but not the basic properties of the lens material.
As a result of plasma treatment, the lens surface becomes ionized, increasing its ability to attract liquids and enhances the wetting angle, resulting in a more hydrophilic lens surface.10 Therefore, after manufacturing, plasma treatment is akin to intense cleaning of the lens, removing impurities from manufacturing, and a lens material’s wettability and interaction with the tear film is improved. This results in reduced fogging and a better visual experience upon application for the patient.
Plasma-treated GP lenses are typically shipped wet in a conditioning solution. In contrast, plasma processing in soft lenses is inherent in the lens material; without it, these materials would be extremely hydrophobic. Applying a plasma coating to soft lenses has been shown to enhance lens surface lubricity, which appears to be the principal contributor to patient comfort.11 However, its effect on GP lens comfort has not been investigated. It is important to note that the ionization does not last forever and that it can be reduced with the use of abrasive cleaners.12
Hydra-PEG. This is a 90% water and polyethylene glycol (PEG) based polymer mixture that is permanently covalently bonded to the surface of the contact lens, effectively creating a wettable surface overlying the lens and separating it from the ocular surface and tear film.13 The optically clear coating encapsulates the core contact lens in a 40nm mucin-like hydrophilic shell without imparting any change to the underlying properties of the lens material.13 PEG has been used in ocular lubricants for decades and has been reported by several sources to improve lens surface wettability, which improves tear breakup time, increases lubricity, reducing friction between the lens and the eyelids and serves to reduce protein and lipid deposition.13-15
 |
|
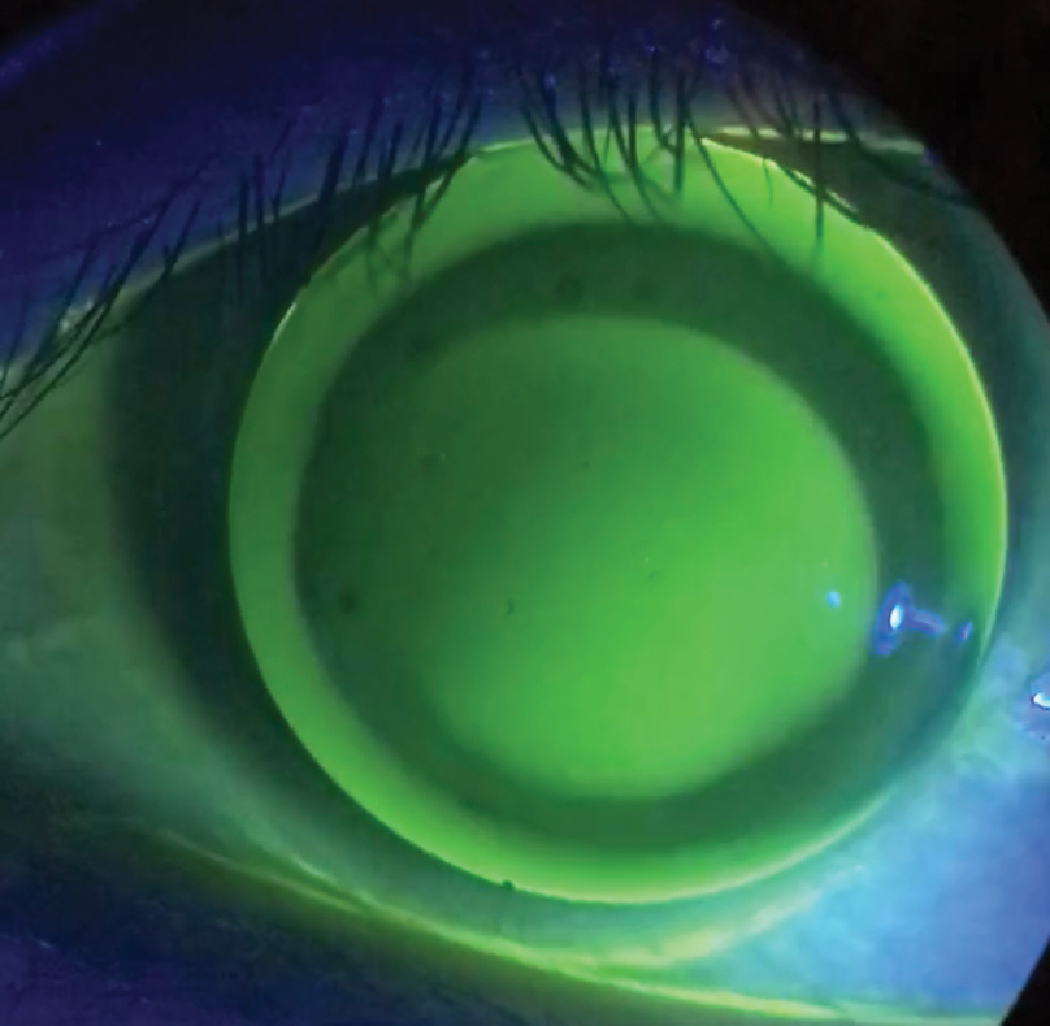
A GP lens with excessive edge clearance, if not fixed, will lead to three and nine o’clock staining and reduced comfort. Click image to enlarge. |
This coating can be applied to all contact lens materials including hydrogel, silicone hydrogel (SiHy) and GPs, including hybrids and sclerals. Currently, there is only one soft contact lens available with Hydra-PEG, SynergEyes’ SimplifEyes 1Day hydrogel daily disposable, which features both a polymer coating on the lens surface and in the packaging solution. Unity Biosync, a SiHy daily disposable coated with Hydra-PEG was distributed by VSP, but is no longer available to practices as of early 2022. SynergEyes also can apply the Hydra-PEG coating to its Duette, UltraHealth and UltraHealth FC hybrid lenses as well as their new SynergEyes iD family of products.
Hydra-PEG is indicated for lens wearers but is especially designed for patients who experience ocular dryness or discomfort associated with contact lens wear, moderate or heavy depositors and scleral lens wearers. A 2020 study comparing lens comfort and dry eye symptoms of dry eye scleral lens wearers fit with Hydra-PEG treated vs. untreated scleral lenses found that patients with Hydra-PEG-treated scleral lenses experienced superior comfort and improved dry eye symptoms, as well a reduction in ocular surface changes and less frequent complaints of foggy vision.16 The study concluded that Hydra-PEG is an effective technology that may improve outcomes for scleral lens wearers with dry eye.16
Additional care considerations exist when prescribing lenses with this coating. A coated lens will be more slippery to the touch and may be more difficult to handle, requiring a brief adjustment period for lens application and removal. Approved cleaners include Boston Simplus (Bausch + Lomb), Unique pH (Menicon), Clear Care and Clear Care Plus with HydraGlyde (Alcon) and Tangible Clean (Tangible Science).17 Buffered, preservative-free, sterile saline is the recommended rinsing agent. All enzymatic, abrasive or alcohol-based cleaners should be avoided as they will damage the coating and reduce its effectiveness.17
The coating can be very durable with proper care but there are factors that will cause the coating to thin over time, which occurs more quickly for some patients than others. This is highly dependent on each patient’s unique ocular environment and include factors such as the severity of their ocular surface disease, whether they are known high depositors and other hostile conditions that impact the front surface. Severe ocular surface disease with cicatricial lid changes/scarring will be abrasive to the lens surface and wear down the coating. Personally, I’ve experienced this with cases of ocular cicatricial pemphigoid, Stevens-Johnson Syndrome and graft-vs. host disease.
Using incompatible solutions, storing lenses dry and rinsing with tap water will also wear down the coating faster, but the coating will remain on the lenses and will continue to provide a more comfortable lens wearing experience than uncoated lenses. For all these reasons, it is impossible to standardize the durability expectation.
In contrast to plasma treatment, Hydra-PEG enhances wettability across the lifespan of the lens if patients follow the care regimen. This can mean a whole 12-month wearing cycle for some patients or less time for others. Patients with a need for specialty lenses may have pathology and conditions that warrant lenses more frequent lens replacement.
Hydra-PEG is expected to last most patients for the natural life of the lens keeping in mind that even normal wear and handling will cause the coating to be thinner at 12 months than at day one. Adding Tangible Boost as a monthly conditioning treatment should enable coated lenses to maintain peak performance longer and allow the patient to have a more reliable wearing experience.
 |
|
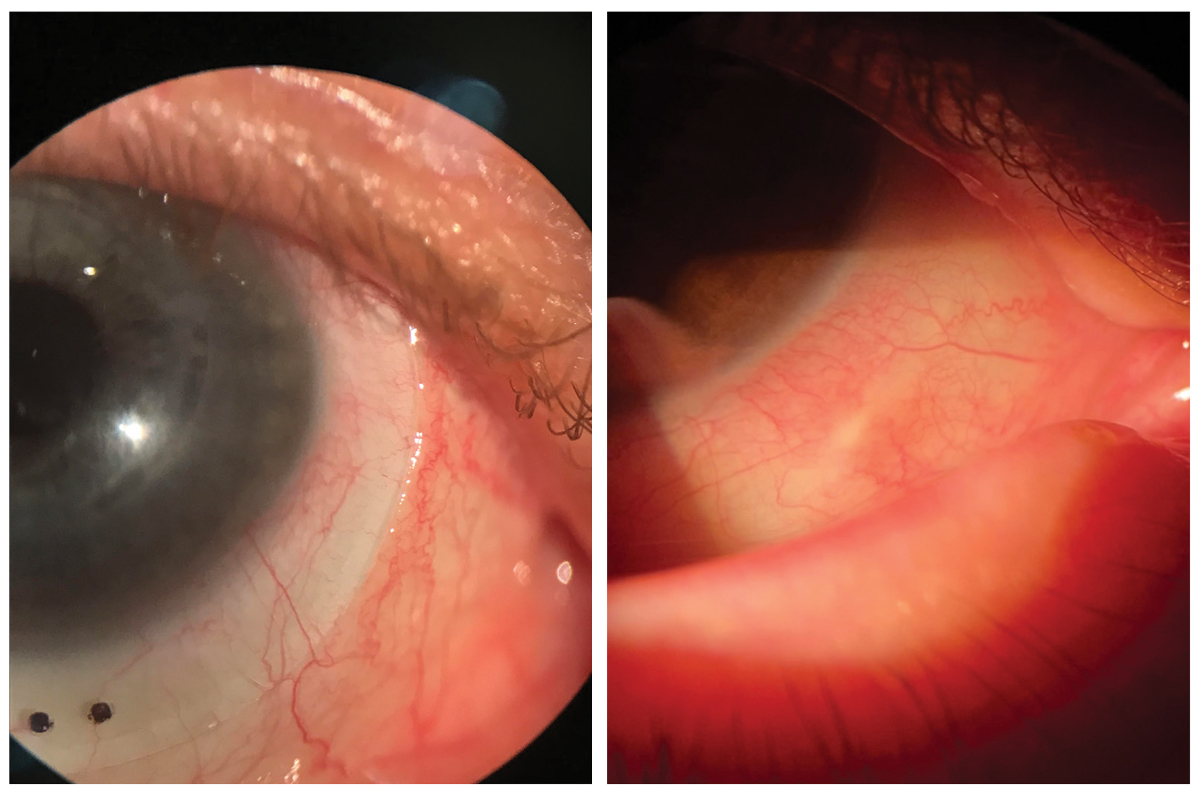
At left, scleral blanching and impingement causing discomfort stemming from scleral misalignment. At right, long-standing impingement can lead to conjunctival hypertrophy and other permanent changes to the tissue, so it’s important that misalignment is addressed during the fitting process. Click image to enlarge. |
Lens Design and Fit
Corneal GPs carry more initial lens awareness than soft lenses or scleral lenses.18,19 However, that doesn’t mean that scleral lens wearers don’t experience discomfort as well—but just like with corneal GPs, the design and/or fit of the lens can also be the culprit.
Corneal GPs. With corneal GPs, the discomfort arises from the interaction between the rigid edge of the lens and the eyelids, particularly the upper lid margin. Edge shape and design are the most important parameters in initial lens comfort.20 The edge should be smooth and well rounded—in contrast, a GP with a defective edge (chipped, abraded, blunt or sharp) the patient will be very aware of the lens with each and every blink, and it will make for quite the negative experience. A well-blended peripheral curve system is preferred to a poorly blended or unblended peripheral curve system that can produce dryness, itchiness and scratchiness.21
Excessive edge-clearance can also be problematic for patient comfort because it funnels in surrounding tears resulting in desiccation and corneal staining at three and nine o’clock on the peripheral corneal regions and it affects the blink quality through increased interaction between the lens edge and the superior lid.22 There is also some evidence that larger GPs are more comfortable for adapted wearers; however, diameter size showed no effect on adaptation of the neophyte wearer.23,24
Although tear exchange is an important aspect in maintaining corneal health, there is little evidence that increasing tear exchange will have a positive effect on lens comfort and, to the contrary, changes to lens parameters that may bring about increased tear exchange (which usually increase lens movement as well) are likely to have a simultaneous negative impact on lens comfort.14
Scleral lenses. In general, due to their larger diameter, these lenses vault over the sensitive innervated corneal tissue, while being filled with fluid. The fact that they rest only on the less sensitive conjunctiva and sclera accounts for their well-accepted comfort by both patients and the practitioners who fit them.
Scleral misalignment occurs during uneven bearing on a scleral lens landing zone and can be a key cause of fit-related patient discomfort. The sclera is often rotationally asymmetric; therefore, lenses that are rotationally symmetric (those with spherical or toric haptics) will not always sit flush with the ocular surface.25 If an edge is loose, a patient will feel it almost immediately due to the friction of the edge with every blink; if an edge is too tight there will be compression and blanching, and in some cases impingement, of the conjunctival tissue under the haptic with corresponding perilimbal injection that worsens and becomes more uncomfortable with increased wear time during the day.
One study compared the performance of spherical and toric scleral lens designs and concluded that toric designs offered a higher comfort rate and increasing wearing times.26 Yet, many studies still cite that discomfort is one of the main reasons, second to handling, as to the reason why a patient may elect to discontinue lens wear.27 Quadrant specific designs may further help to improve comfort by improving scleral alignment.28
The Scleral Shape Study Group reported that a relatively small percentage of eyes are described as regularly toric (28.6%), 40.7% as asymmetrical toric and 26% as irregular toric.29 Other design modifications, such as vaults, lifts, microvaults, channels and notches have helped improve the ability to fit sclerals over even the most unusual ocular shapes by allowing the lens to align better with various scleral elevations (pterygiums, pingueculae, blebs, etc.). This results in enhanced comfort and a better physiological response of the ocular surface for the wearer. Scleral lens customization continues to advance in an effort to improve vision and comfort for the wearer as more research evolves about scleral shape.
Takeaways
Contact lens materials and designs have evolved immensely over the past few decades and prescribing newer lenses and adding Hydra-PEG to GP materials can potentially help practitioners address common problems. Newer contact lens materials are intended to improve ocular surface biocompatibility, and designs intended to improve fit, comfort and visual performance are also emerging. It is beneficial to stay abreast of the novel innovations and technologies in lens materials and designs to offer the best to patients.
Unfortunately, only a certain degree of improvement in patient comfort can be obtained by optimizing lens surface treatments and designs. It is incumbent upon optometrists to identify individuals at risk for contact lens discomfort. When identified, it is critical to appropriately treat the ocular surface and provide an environment conducive to comfortable long-term contact lens wear.
Optometrists need to understand and appreciate the effects of the ocular surface and how it can influence contact lens wear. A healthy ocular surface will not guarantee a successful wearing experience but will maximize the chances of one occurring.
With the ocular surface, critical clinical consideration should be made to the health of the lid margins, conjunctiva, cornea, tear film and all glands involved in producing the tear film. It is with the proactive treatment of the ocular surface and optimization of the tear film that practitioners will be able to help support the new technology of lenses that are being fit today.
1. Nichols JJ, Jones L, Nelson JD, et al. The TFOS international workshop on contact lens discomfort: introduction. Invest Ophtalmol Vis Sci. 2013;54(11):TFOS1-6. 2. Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013;39(1):93-9. 3. Sulley A, Young G, Hunt C, et al. Retention rates in new contact lens wearers. Eye Contact Lens. 2018;44 Suppl 1:S273-82. 4. Stapleton F, Tan J. Impact of contact lens material, design and fitting on discomfort. Eye Contact Lens. 2017;43(1):32-9. 5. Bennett ES, Henry, VA. Clinical Manual of Contact Lenses 4th Edition. Philadelphia, PA: Wolters Kluwer Medical; 2014. 6. Bennett ES. Gas permeable material selection. In: Bennett ES, Henry VA, eds. Clinical Contact Lens Practice. Philadelphia, PA: Lippincott Williams & Wilkins; 2014:89-103. 7. Feldman G, Yamane SJ, Herskowitz R. Fluorinated materials and the Boston Equalens. Cont Lens Forum. 1987;12:57. 8. Walker J. A clinical and laboratory comparison of the deposition characteristics of both silicone/acrylate and fluoro-silicone/acrylate lenses. J Br Contact Lens Assoc. 1988;11(S:1988):83-6. 9. Jang JK, Shin HS. The effects of plasma surface treatment on fluorosilicone acrylate RGP contact lenses. J Korean Ophthalmic Opt Soc. 2010;15(3):207-12. 10. Bergmann M, Ledernez L, Dame G, et al. Nanofilms produced by magnetron enhanced plasma polymerization from methane and oxygen for coating of rigid contact lenses. Plasma Process Polym. 2013;10:970-7. 11. Vidal-Rohr M, Wolffsohn JS, Davies LN, Cervino A. Effect of contact lens surface properties on comfort, tear stability and ocular physiology. Cont Lens Anterior Eye. 2018;41(1):117-21. 12. Gu ZW, Han Y, Pan FS, et al. Surface hydrophilicity improvement of RGP contact lens material by oxygen plasma treatment. Mater Sci Forum. 2009;610-613:1268-72. 13. Sindt CW. Tangible Hydra-PEG: A novel custom contact lens coating technology designed to improve patient comfort and satisfaction. 2016. www.eye-iq.com/uploads/hydra-peg-white-paper.pdf. Accessed July 1, 2022. 14. Jones L, Brennan NA, Gonzalez-Meijome J, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the contact lens materials, design and care subcommittee. Invest Ophthalmol Vis Sci. 2013;54(11):TFOS37-70. 15. Ousler GW, Michaelson C, Christensen MT. An evaluation of tear film breakup time extension and ocular protection index scores among three marketed lubricant eye drops. Cornea. 2007;26(8):949-52. 16. Mickles CV, Harthan JS, Barnett M. Assessment of a novel lens surface treatment for scleral lens wearers with dry eye. Eye Contact Lens. 2021;47(5):308-13. 17. Gorman R. The eight most common Tangible Hydra-PEG questions. Tangible Science. tangiblescience.com/blogs/care-tips/8-common-questions. Accessed July 1, 2022. 18. Fonn D, Gauthier CA, Pritchard N. Patient preferences and comparative ocular responses to rigid and soft contact lenses. Optom Vis Sci. 1995;72(12):857-63. 19. Shorter E, Schornack M, Harthan J, et al. Keratoconus patient satisfaction and care burden with corneal gas-permeable and scleral lenses. Optom Vis Sci. 2020;97(9):790-6. 20. Edwards K. Rigid gas-permeable contact lens problem solving. Optician. 2000;219(5740):18-24. 21. Picciano S, Andrasko GJ. Which factors influence RGP lens comfort? Optom Today. 1989;4(5):31-3. 22. Schnider CM, Terry RL, Holden BA. Effect of patient and lens performance characteristics on peripheral corneal desiccation. J Am Optom Assoc. 1996;67(3):144-50. 23. Williams-Lyn S, MacNeill K, Fonn D. The effect of RGP back optic zone radius and diameter changes on comfort. Int Contact Lens Clinic. 1993;20:223-118. 24. Debarun D, Wolffsohn J. Effect of large diameter and plasma coating on the initial adaptation of gas permeable contact lens fitting for neophytes. Cont Lens Anterior Eye. 2021;44(1):76-80. 25. Ritzmann M, Caroline PJ, Börret R, Korszen E. An analysis of anterior scleral shape and its role in the design and fitting of scleral contact lenses. Cont Lens Anterior Eye. 2018;41(2):205-213. 26. Visser ES, Visser R, Van Lier HJJ. Advantages of toric scleral lenses. Optom Vis Sci. 2006;83(4):233-6. 27. Macedo-de-Araújo RJ, van der Worp E, González-Méijome JM. A one-year prospective study on scleral lens wear success. Cont Lens Anterior Eye. 2020;43(6):553-61. 28. Barnett M, Carrasquillo K, Schornack M. Clinical outcomes of scleral lens fitting with a data-driven, quadrant-specific design: multicenter review. Optom Vis Sci. 2020;97(9):761-5. 29. DeNaeyer G, Sanders DR, van der Worp E, et al. Qualitative assessment of scleral shape patterns using a new wide field ocular surface elevation topographer: the SSSG Study. J Cont Lens Res Sci. 2017;1(1):12-22. |