Zoom in on Contact LensesThis August issue is our 46th annual contact lens report, where we help you use new and old techniques to improve your fitting skills.
|
With the multitude of soft contact lens technologies and options available to our patients, how do you choose which contact lens to prescribe for a new wearer? While many patients may seek out contact lenses to eliminate their need or reduce their dependency on glasses, there are several important factors to consider, improving their success with these medical devices. Contact lens materials, optics and replacement schedules are important considerations to enhance patient comfort, ocular health, vision and ultimately lens retention for new wearers.
Where to Start?
Like many ocular conditions, prescribing contact lenses begins with a good case history. Getting to know your patients’ lifestyle, visual demands, occupation and hobbies are all vital in recommending appropriate contact lens wear and replacement schedules. For example, someone who has the goal of being glasses-free on the weekends might be better suited with a daily disposable lens as opposed to someone who prefers to wear contact lenses every day, who may do well with daily, biweekly or monthly replacement schedules.
Although many practitioners tend to steer away from recommending overnight wear, some occupational demands might warrant flexible or extended wear, such as for firefighters or on-call medical professionals. Selecting an approved contact lens for extended wear and educating patients on proper lens wear, care and follow-up are essential.
Ocular and systemic health are also important aspects of case history to investigate. There are contact lens replacement schedules and material considerations for patients with ocular allergies and dry eye disease. Systemic medications can exacerbate some of these ocular conditions as well. For many of these patients, daily replacement of contact lenses may be beneficial to optimize ocular health and comfort.
Setting realistic expectations for vision correction is also important prior to contact lens fitting, particularly for presbyopes. Determining the type of vision correction patients prefer (distance only with reading glasses, monovision correction, multifocal contact lenses) up front can save a lot of chair time and help with initial lens selection. Every patient at each visit requires repeated step-by-step care and handling instructions including how their underlying or associated ocular and systemic conditions may impact their contact lens wear schedule.
 |
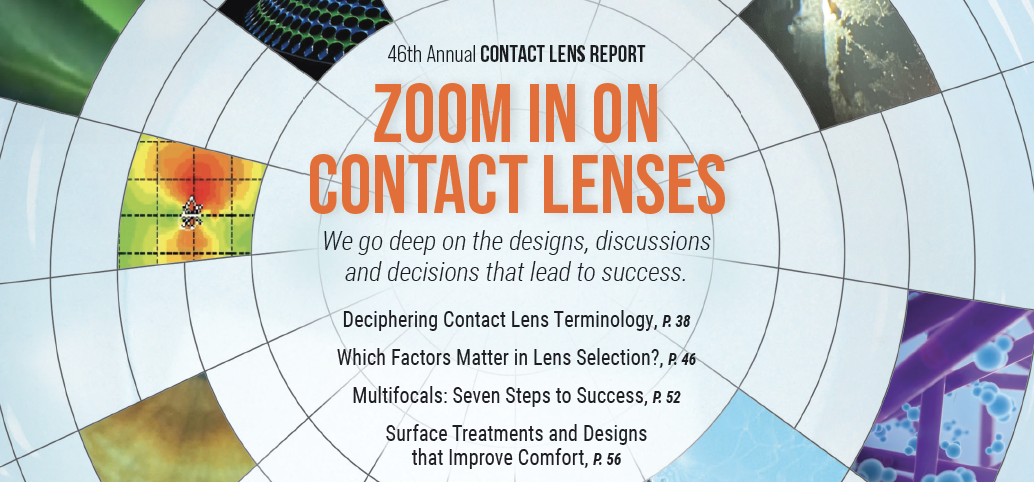
| Fig. 1. Noninvasive tear breakup time as measured by the Oculus Keratograph. This patient’s first time measured at 2.48 seconds with an average of 6.83 seconds. Click image to enlarge. |
Cornea Shape and Pupil Size
The patient’s refractive error and corneal/scleral shape will often guide initial lens selection. Corneal and scleral shape can be measured using corneal tomography and corneoscleral profilometry. There are several profilometers available, and depending on the instrument used, scleral data points up to 22mm onto the sclera with up to 10µm of accuracy can be measured. This technology is beneficial to help design gas permeable (GP), hybrid, scleral, orthokeratology and custom soft lenses. By further understanding the scleral asymmetry, a best-fit lens can be designed to fit the contour of the ocular surface more precisely.1 Higher refractive errors, >±4.00D, should be vertexed back to the corneal plane, and initial power should be selected and troubleshooted based on the fitting guide, especially for multifocal lens designs. Determining the dominant eye and near add power are important when fitting contact lenses for patients with presbyopia.
Pupil size also plays an important role when fitting multifocal lenses. Many soft and specialty multifocal lenses use the concept of simultaneous vision, with concentric aspheric rings of distance, intermediate and near focus to allow for acceptable range of vision. They may use distance center or near center designs. In order for the multifocal lens to sufficiently achieve the power distribution needed to meet the visual demands of the patient, the pupil must be large enough (between 3mm and 5mm depending on the add power for soft lenses) to cover these multiple zones.2 However, if the pupil is too large (5mm), patients may experience light distortion.3
If the patient’s vision is not sufficient with a simultaneous vision design, an extended depth-of-focus design, a translating GP multifocal or a specialty lens with the ability to change the multifocal zone size may be a better fit. Some custom lenses are also available with decentered optics to better align the optical center with the pupil center.
Corneal curvature may be measured with a keratometer, and pupil size and horizontal visible iris diameter (HVID) may be measured via various methods (manual vs. automated). Many practitioners use topographers, tomographers and even profilometers to help determine several factors that are beneficial when selecting a contact lens design: regular vs. irregular astigmatism, pupil size, HVID, keratometry (K) readings, eccentricity, apical centration, scleral toricity and topography and sagittal height.
A cornea that is smaller or larger than average (average HVID is about 11.8mm and ranges from 11.6mm to 12.0mm), flatter (<42.00D) or steeper (>47.00D) than average or has more corneal astigmatism and/or scleral toricity may do better with specialty contact lens designs to improve lens centration and patient comfort.4 Scleral asymmetry increases as you move away from the limbus. The nasal quadrant of the sclera is flatter than the temporal quadrant, and the sclera has a tangent profile.5,6 Patients who have conjunctival irregularities (e.g., pinguecula, cysts) may need specialty lenses to help improve vision, comfort and centration.
 |
| Fig. 2. Meibography of the right lower meibomian glands showing atrophy, dilation and truncation of the glands. Click image to enlarge. |
Picking Base Curves
Many readily manufactured “boxed” soft contact lenses are only available in one diameter and one or two base curve (BC) parameters. The flexibility of soft lens materials allows them to be fit on many patients with a variety of corneal measurements (almost one-size-fits-all), but if there is a choice between BCs, flatter K readings will do well with a flatter BC, and steeper K readings will do well with a steeper BC. However, if the lens is well-centered, provides full coverage over the limbus and moves an appropriate amount to allow tear film exchange for optimal corneal health, most patients will do well in the limited diameter and BC choices of each company.
If the lens is fitting tight or loose, a flatter or steeper BC, respectively, within the same lens brand and design can be trialed if available. Changing diameter or BC between different brands, or between lens designs within the same brand, may not change the fit in a predictable fashion due to variations in material, water content and modulus.
Another approach to lens selection, rather than considering corneal curvature to pick an initial BC, is to evaluate sagittal depth data to select a lower or higher sagittal height lens that may better match the corneal shape to result in an acceptable fit. Not all soft lenses perform the same way on the eye due to their sagittal depth. When you increase the diameter of the lens, you also increase the overall sagittal depth of the lens.7 Increasing the sagittal depth of the lens also reduces lens movement and may help improve overall comfort.7
In a recent study, 44 lens designs of different daily disposable, two-week replacement, four-week replacement and toric lenses were evaluated for contact lens sagittal height and ranged from 3,372µm to 4,157µm.8 This shows that selecting or changing lenses based on BC alone may not be most appropriate as sagittal height varies between lenses and can have an impact on lens fit.
 |
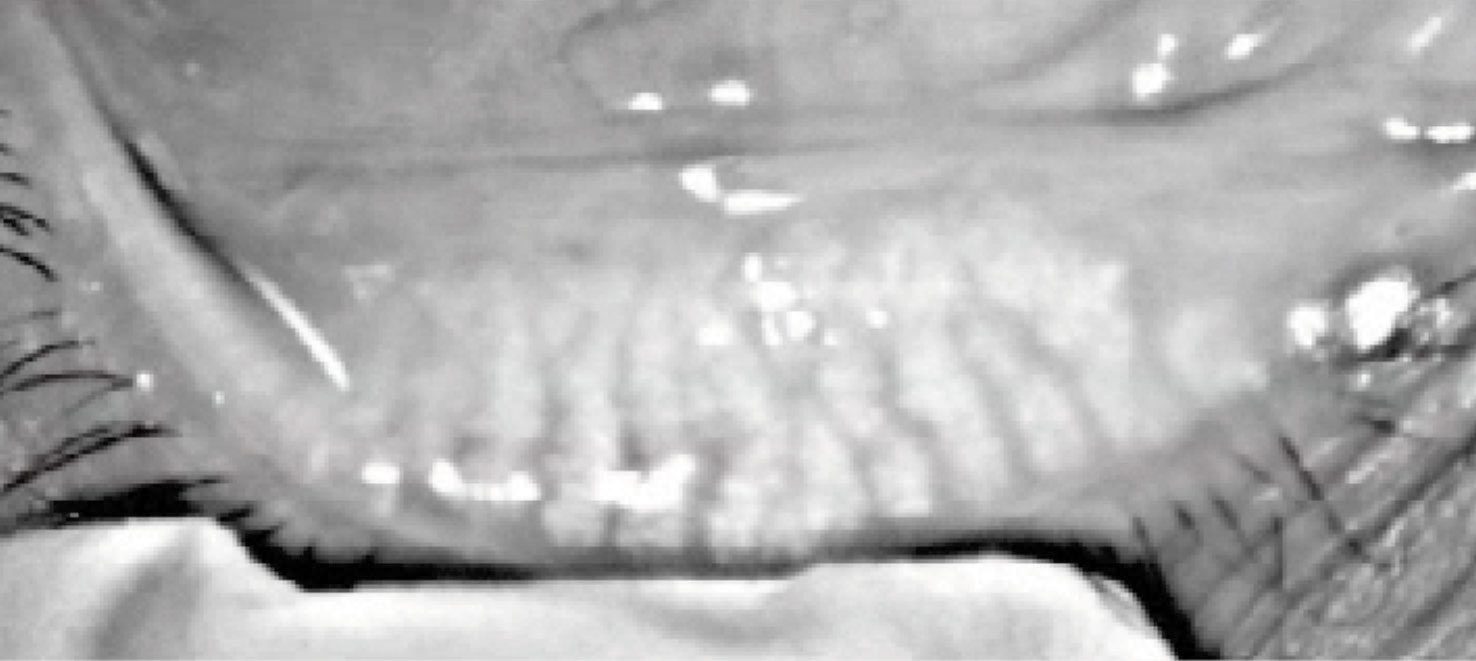
| Fig. 3. Eversion of the upper and lower eyelids reveals mild papillae of the palpebral conjunctiva in each eye. Click image to enlarge. |
Impact of Dry Eye
Ocular surface disease, specifically dry eye disease, is one of the leading causes of contact lens dropout. Performing a thorough slit lamp examination and dry eye evaluation may prevent future contact lens dropouts by addressing ocular health issues prior to lens fitting. Paying close attention to the eyelids, lashes and tear film can facilitate more successful contact lens wear. Inflammation from conditions such as blepharitis and meibomian gland dysfunction should be managed prior to fitting contact lenses. Upper and lower lid eversion is beneficial to rule out papillary reactions and lid wiper epitheliopathy that may lead to contact lens intolerance.
Examination of the cornea for scarring, neovascularization and active inflammation can provide insight into previous lens wear habits and ocular surface conditions, as well as guide lens material selection and patient education to maximize compliance. When evaluating for dry eye disease, instruments that measure noninvasive tear breakup time, tear meniscus height, conjunctival hyperemia and meibomian gland atrophy may be helpful (Figures 1 and 2).
Use sodium fluorescein to assess corneal staining and evaluate invasive tear breakup time. However, some practitioners prefer to not use sodium fluorescein during the contact lens fitting visit to prevent staining the soft contact lens yellow.
Once the ocular surface condition is stabilized, these patients will benefit from daily disposable lenses. In some cases, hydrogel lenses can provide increased comfort for patients with ocular surface disease due to higher water content. Also, there are silicone hydrogel lenses that have a water gradient to improve the tear film interaction with the contact lens surface.
Materials
This important factor enhances patient comfort and maintains ocular health. Material properties to be considered include sufficient oxygen transmission, good wettability and resistance to deposits. Each material has its advantages and disadvantages and should be carefully selected based on the patient’s needs. Hydrogel contact lenses traditionally contain high water content, allowing oxygen to pass through the lens and are often a good option for patients with dry eye disease. However, these lenses tend to attract more protein deposits.9 Secondary to this, hydrogel lenses should be replaced more frequently and digitally rubbed with cleaner more regularly.
Contact lenses made from silicone hydrogel (SiHy) materials allow more oxygen to reach the cornea compared with regular hydrogel lenses. These lenses are great for patients who need extended wear replacement schedules. SiHy lenses are often easier to handle for new wearers during application and removal training as they are slightly firmer compared with hydrogels. SiHy contact lenses tend to attract more lipid deposits and have decreased wetting compared with hydrogel lenses. Subsequently, many manufacturers have added various wetting agents to SiHy lenses to keep the lenses more comfortable for longer periods of time.10
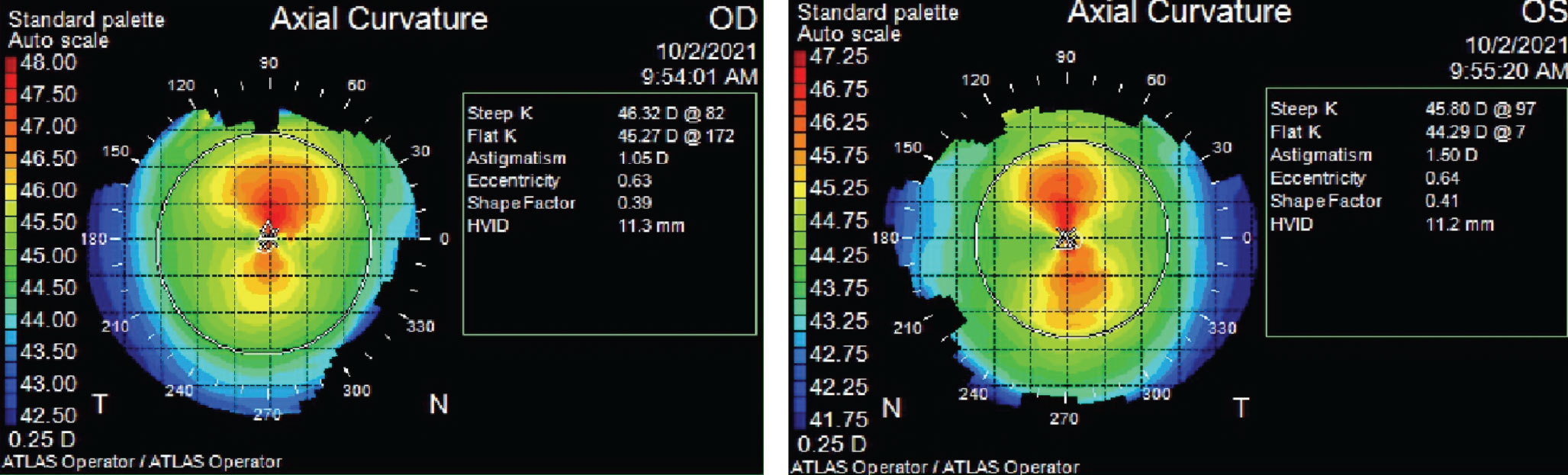 |
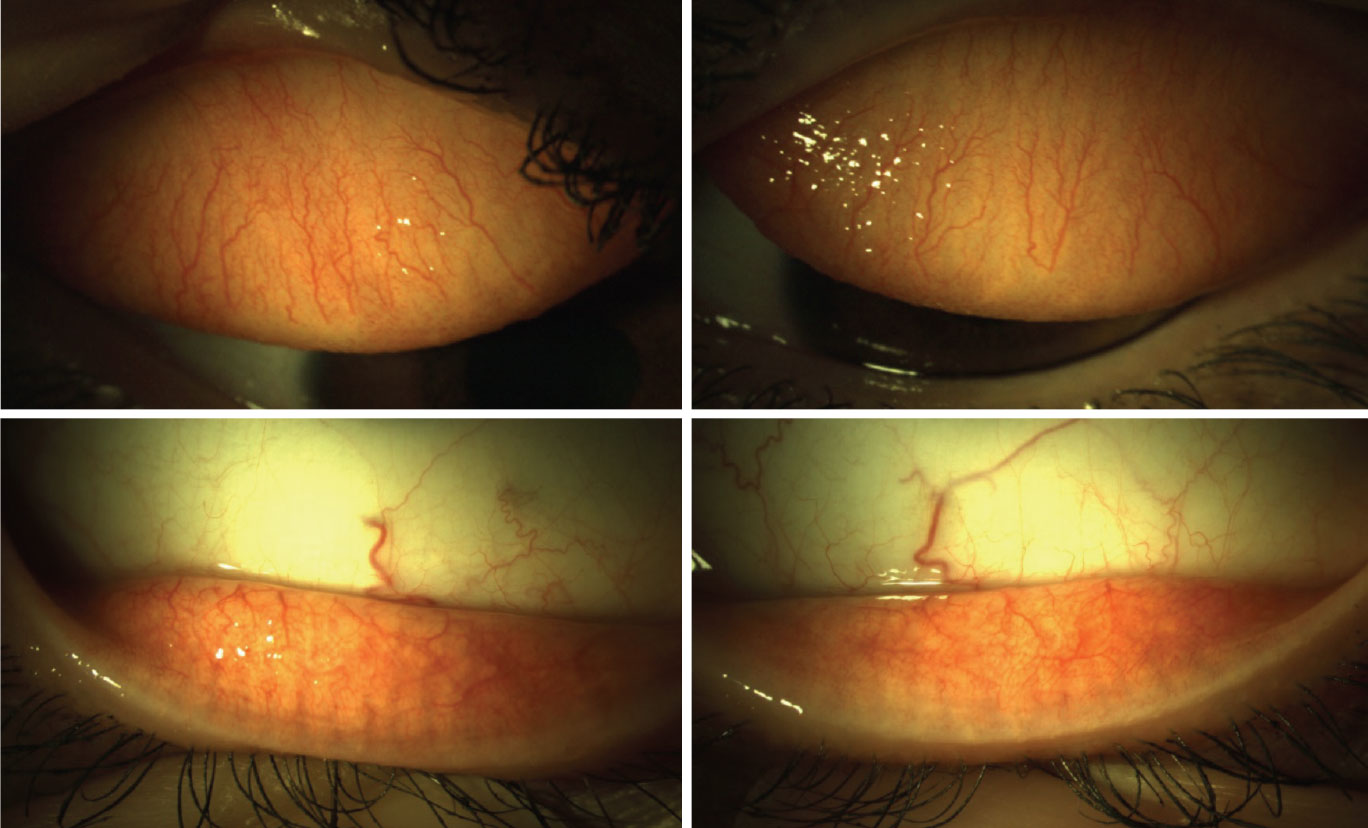
| Fig. 4. Zeiss Atlas axial topography maps of both eyes show smaller-than-average HVID measurements and steeper-than-average K readings. Click image to enlarge. |
Case 1: Allergies
A 17-year-old male presented with complaints of decreased vision at distance, problems seeing the board at school and driving. His medical history was remarkable for allergies, and he took over-the-counter antihistamines when needed. He reported mucus discharge for the past two weeks. He had worn contact lenses in the past but discontinued them due to discomfort. His goal was to wear contact lenses again.
We’ve all had patients like this present to our offices. Secondary to his complaints, eversion of his eyelids would be important to monitor for a papillary reaction, and he would be a great candidate for daily disposable contact lenses (Figure 3).
Case 2: Small HVID
A 22-year-old female presented with the goal of being less dependent on glasses and was motivated to wear contact lenses daily. She denied any systemic or ocular conditions, including no symptoms of dryness or allergies. Her slit lamp examination was unremarkable. She had a moderate compound myopic astigmatism refractive error OU.
She trialed several soft toric contact lenses in different brands, materials and diameters (ranging from 14.3mm to 14.5mm) that did not result in acceptable comfort or fit. Looking at her smaller-than-average HVIDs (11.3mm OD, 11.2mm OS) and steeper-than-average K readings in the topography images explains why (Figure 4).
Average HVID is about 11.8mm, and a patient with a corneal size that falls outside of the 11.6mm to 12.0mm range may be a good candidate for a custom soft lens.4 This patient would do well with a monthly or quarterly replacement custom soft toric lens design (OD BC 7.9mm, diameter 14.2mm; OS BC 8.0mm, diameter 14.3mm based on the fitting guide) to improve her overall comfort and fit of the contact lenses.
Custom soft contact lenses are fit empirically; the minimum data needed includes manifest refraction, K readings and HVIDs, but corneal topography/tomography maps or profilometry scans can aid in a more customized fit looking at sagittal height data. The first lenses are ordered via a fitting guide or calculator, or through the company’s consultation department. Initial chair time is reduced by ordering empirically rather than diagnostically. Because the lenses are custom-made based on the patient’s measurements, these soft toric lenses can often be finalized after one to two follow-up visits.11
Case 3: Multifocals
A 61-year-old female presented with the chief complaint of poor near vision with her current contact lenses. She had been wearing daily disposable monovision contact lenses, OD dominant set for distance/OS effective add of +1.50D, for about 15 years but was recently having trouble reading small numbers on her printed spreadsheets at work. She had no issues with distance or computer vision tasks. She was motivated to try any options to prevent the need for reading glasses over contact lenses and was refit into a daily disposable multifocal lens design, which resolved her symptoms.
Although some practitioners may be hesitant to switch a patient from monovision to multifocal lens designs, the benefits of binocularity and increased range of vision (distance, intermediate and near) should be considered. Advances in technology have allowed us to offer more options for our patients with presbyopia. Even patients who have worn monovision for years can adapt successfully to multifocal optics.
Takeaways
Every new contact lens wearer needs to be managed individually. Assess their needs, motivation for contact lens wear, ocular and systemic health and corneal parameters. Completing a thorough assessment and prescribing a specific contact lens for their individual needs can set them and the practitioner up for success.
Dr. Harthan is a professor at the Illinois College of Optometry and chief of the Cornea Center for Clinical Excellence at the Illinois Eye Institute. She has received fees from Allergan, Essilor, Euclid, the International Keratoconus Academy, Kala, Metro Optics and SynergEyes. Dr. Man is an assistant professor at the Illinois College of Optometry and specialty care educational coordinator at the Illinois Eye Institute. She has no financial disclosures. Both are Fellows of the American Academy of Optometry and Scleral Lens Society.
1. Noyes M. Scleral topography: measuring and matching its shape. RCCL. 2021;158(4):18-22. 2. Papdatou E, Del Aguila-Carrasco AJ, Esteve-Taboada D, et al. Objective assessment of the effect of pupil size upon the power distribution of multifocal contact lenses. Int J Ophthalmol. 2017; 10(1):103-108. 3. Monsálvez-Romín D, González-Méijome JM, Esteve-Taboada JJ, García-Lázaro S, Cerviño A. Light distortion of soft multifocal contact lenses with different pupil size and shape. Cont Lens Anterior Eye. 2020;43(2):130-6. 4. Caroline PJ, Andre MP. The effect of corneal diameter on soft lens fitting, part 1. Contact Lens Spectrum. April 1, 2002. www.clspectrum.com/issues/2002/april-2002/contact-lens-case-reports. Accessed July 1, 2022. 5. van der Worp E, Graf T, Caroline P. Exploring beyond the corneal borders. Contact Lens Spectrum. June 1, 2010. www.clspectrum.com/issues/2010/june-2010/exploring-beyond-the-corneal-borders. Accessed July 1, 2022. 6. van der Worp E, Bornman D, Lopes Ferreira D, et al. Modern scleral contact lenses: a review. Cont Lens Anterior Eye. 2014;37(4):240-50. 7. Young G. Ocular sagittal height and soft contact lens fit. Cont Lens Anterior Eye. 1992;15(1):45-9. 8. van der Worp E, Lampa M, Kinoshita B, et al. Variation in sag values in daily disposable, reusable and toric soft contact lenses. Cont Lens Anterior Eye. 2021;44(6):101386. 9. Gromecki S. Contact lens care: soft contact lens deposition-part I. Contact Lens Spectrum. February 1, 2006. www.clspectrum.com/issues/2006/february-2006/contact-lens-care. Accessed July 1, 2022. 10.Bennett ES, Henry VA. 5th Edition. Philadelphia, PA: Wolters Kluwer Medical; 2020. 11. de Brabander J, Brinkman CJ, Nuyts RM, et al. Clinical evaluation of a custom-made toric soft lens. Cont Lens Anterior Eye. 2000;23(1):22-8. |