 |
Q:
I am seeing a one-day post-op cataract patient that has moderate corneal edema, mild discomfort, and an IOP of 40mm Hg. What should I do?
A:
To answer this timely question, I’ve asked Brian Den Beste, OD, and his son Kyle Den Beste, MD, to respond. The father-son team work at Den Beste Eye Consultants in Orlando.
“I think it’s appropriate to explain why this happens,” says Kyle Den Beste, MD, a cornea and cataract surgeon. “Some patients are just prone to have elevated postoperative pressures, usually because their trabecular meshwork is compromised.”
However, the majority of patients have a pressure spike because of retained viscoelastic material. Like all surgeons, he uses viscoelastic compounds during cataract surgery for a host of reasons, but most often to protect the corneal endothelium during phacoemulsification. “The compound is invisible and despite our best efforts to remove all of it, sometimes a small amount gets left behind in the angle and blocks aqueous outflow,” Dr. Den Beste notes.
 |
|
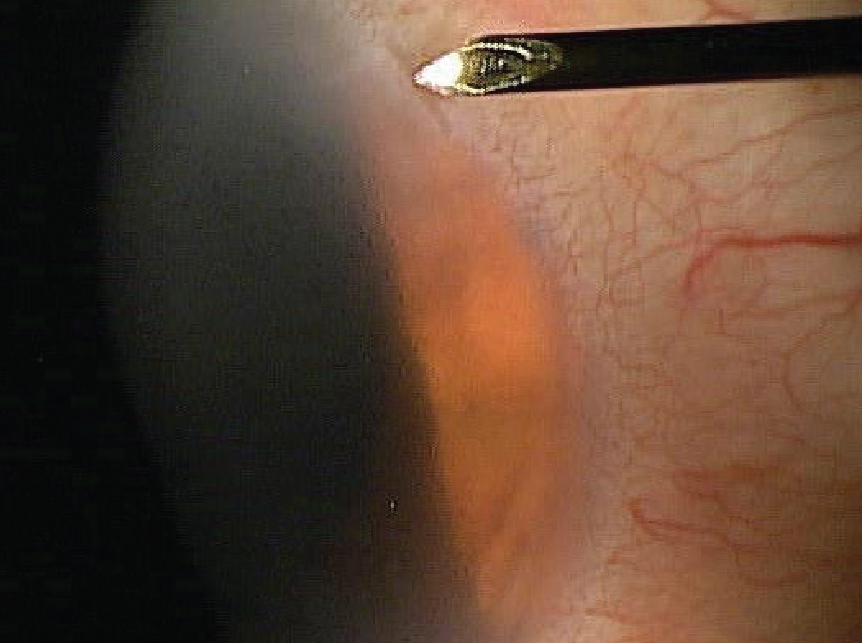
With a spud, place pressure on the conjunctival side of the paracentesis incision. Photo: Howell Findley, OD. Click image to enlarge. |
To safely lower pressures that are 35mm Hg or under, Brian Den Beste, OD, will typically increase the topical steroid dosage and add either timolol or timolol/dorzolamide in combination, because the intraocular pressure (IOP) elevation is from both a mechanical and an inflammatory process. “If the IOP is above 35mm Hg, we typically burp the wound,” he says.
“I always tell optometrists that comanagement of post-op care is great for patients, but in instances like this if the referring doctor is not comfortable with lowering the pressure, there is no shame in sending the rare patient back for a burping,” Kyle Den Beste, MD, points out.
Having worked with Orlando area optometrists for over 35 years, Brian Den Beste, OD, has always been impressed with not only their compassion to learn but also their total commitment to patient safety. “I have burped many incisions over the years without complication, as have a number of my colleagues, but not everyone feels comfortable with the technique,” he notes.
Procedure of Choice
Burping incisions is relatively simple and done at the slit lamp. Controlling the lids with your off hand is key. Just like in foreign body removal, start with three drops of proparacaine and a drop of antibiotic. Some pretreat the eye with Betadine (povidone-iodine 5%).
Kyle Den Beste, MD, recommends applying pressure with a blunt instrument adjacent (toward the sclera) to the paracentesis wound as you observe the aqueous outflow. The wound is like a trap door and mild pressure on the outside of the wound allows a quick escape of fluid.
“The instrument the two of us prefer is called an Ellis Spud,” says Brian Den Beste, OD. “I use it for foreign body and rust ring removal.”
The spud works like a small spoon, and its back side makes a perfect smooth tool to apply pressure to the trap door incision. Some prefer a 30-gauge needle or anything with a flat surface.
Be prepared that some incisions may be harder to burp than others. If that is the case, Dr. Den Beste will go to the main wound to achieve the necessary pressure relief.
Once the procedure is complete, perform a quick IOP check to ensure a safe pressure has been achieved. Often the IOP will drop from over 40mm Hg to 12mm Hg instantaneously. We apply a drop of antibiotic, and typically see the patient back in two to three days. It’s rare to observe a subsequent elevated IOP, but it happens on occasion.
“Patients with discomfort feel immediate relief, and it’s amazing how quickly microcystic corneal edema resolves,” Kyle Den Beste, MD, says. “Still, in patients that are more at risk, such as those with pre-existing glaucoma, we are more aggressive with prescribing pressure medications or short-term oral acetazolamide."
Dr. Ajamian is board certified by the American Board of Optometry and serves as Center Director of Omni Eye Services of Atlanta. He is vice president of the Georgia State Board of Optometry and general CE chairman of SECO International. He has no financial interests to disclose.

