 |
An 18-year-old Hispanic male presented with acute onset pain, redness, photophobia and loss of vision in the left eye. His medical, ocular and family histories were all unremarkable, and he was not taking any over-the-counter, prescription or illicit medications.
Entering visual acuity (VA) was 20/60 OD with pinhole improvement to 20/40 and 20/200 with pinhole improvement to 20/100 OS. Extraocular motilities were full, confrontation visual fields were full and there was no relative afferent pupillary defect. IOP was 21mm Hg OD and 16mm Hg OS by applanation. Anterior segment exam was unremarkable OD. Regarding the left eye, there was 2+ diffuse conjunctival injection, the anterior chamber was deep, there were 4+ mixed pigment, red blood cells and white blood cells circulating in the anterior chamber, and there was a 1.6mm hyphema settled inferiorly. Posterior segment imaging is included here for review.
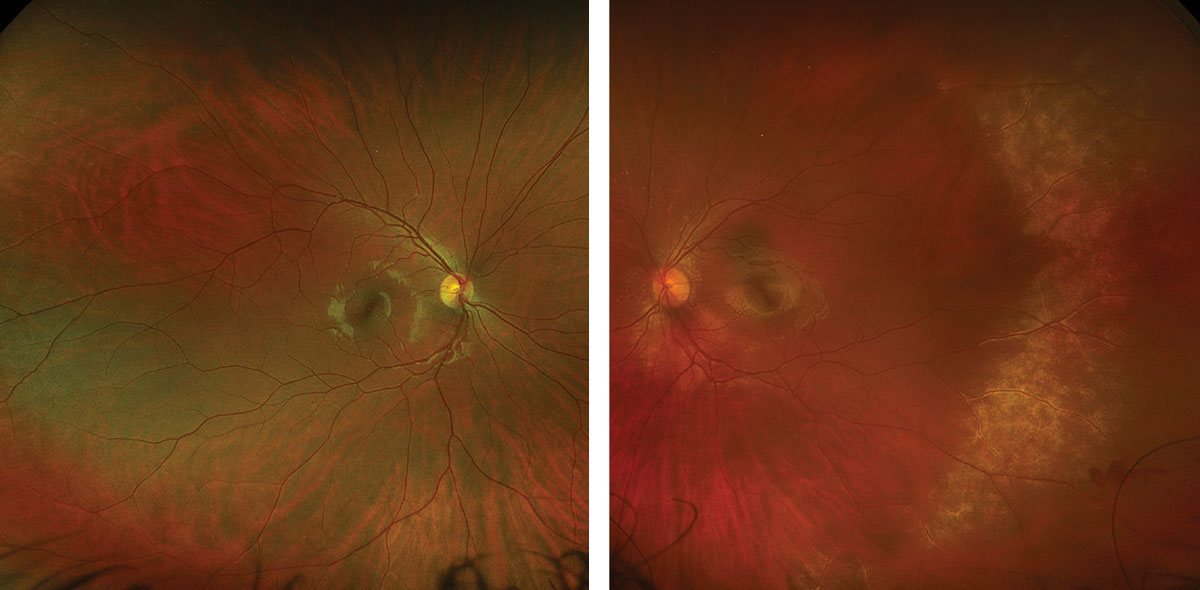 |
Figs. 1 and 2. Optos ultra-widefield fundus photo of the right eye (left) and left eye (right). Click image to enlarge. |
Take the Retina Quiz
1. How would you interpret the OCT of the left eye?
a. There is full-thickness retinal hyperreflectivity.
b. There is hyperreflectivity and disruption of the photoreceptor and retinal pigment epithelial (RPE) layers.
c. There is inner retinal thickening and hyperreflectivity.
d. All of the above are applicable.
2. What is the most likely diagnosis for this patient?
a. Commotio retinae.
b. Purtscher retinopathy.
c. Susac syndrome.
d. Viral retinitis.
3. Which of the following is the most appropriate management of this patient’s posterior segment findings?
a. Emergent stroke work-up.
b. Intravitreal anti-VEGF injection.
c. Intravitreal tap with combined ganciclovir and foscarnet injections.
d. Serial dilated fundus examinations with scleral depression.
4. Which of the following best describes the pathophysiology of this patient’s retinopathy?
a. It is infectious in nature.
b. It is inflammatory in nature.
c. It is ischemic in nature.
d. It is traumatic in nature.
5. All of the following regarding the posterior segment findings are true, except:
a. The disease is self-limiting.
b. Vision may recover to, or near, baseline levels.
c. In the absence of systemic treatment, there will likely be fellow eye involvement within a few days.
d. All of the above are true.
Diagnosis
The patient was Shafer negative without vitreous hemorrhage OU. The fundus was normal OD, but there was a large area of retinal whitening temporally with adjacent pre-retinal hemorrhage, as well as peripapillary and subtle macular whitening OS (Figures 1 and 2). There were no retinal breaks seen with careful peripheral examination or B-scan ultrasound.
Differential diagnoses for retinal whitening should include commotio retinae, retinal ischemia, Purtscher or Purtscher-like retinopathy, chronic retinal detachment and retinitis. Further questioning revealed he suffered trauma while working at a gym from an elastic band that struck his left eye two and a half hours prior to examination.
The patient was diagnosed with a traumatic grade I hyphema, iritis, commotio retinae and preretinal hemorrhage OS. He was started on topical prednisolone acetate 1% six times daily and cyclopentolate 1% three times daily in the left eye. He was initially monitored every one to two days during the rebleed period to ensure that any secondary ocular hypertension could be identified and treated promptly if present. Additional recommendations included bed rest, sleeping with the head of his bed elevated, avoiding oral non-steroidal anti-inflammatory drugs/blood thinners, ice packs as needed for comfort and acetaminophen as needed for pain.
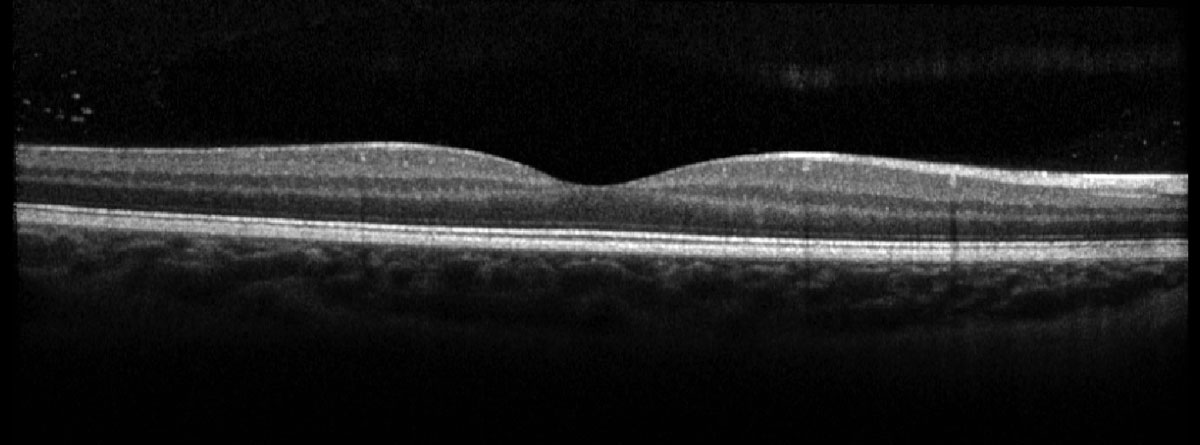 |
Fig. 3. Heidelberg OCT of the right macula. Click image to enlarge. |
 |
|
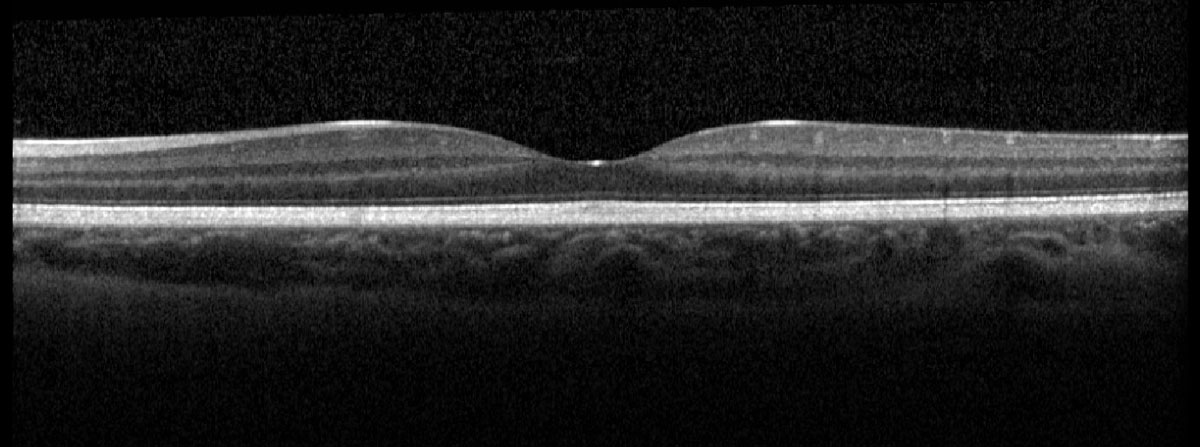
Fig. 4. Heidelberg OCT of the left macula. Click image to enlarge. |
Discussion
Commotio retinae is a common post-traumatic fundus finding secondary to closed-globe blunt trauma that was first described by Berlin in 1873.1,2 The term “Berlin edema” is also used to describe commotio retinae, but typically refers to involvement of the posterior pole. Closed-globe blunt trauma often produces a coup-contrecoup force that can produce commotio retinae at the site of direct scleral impact (coup trauma) or opposite the site of direct impact (contrecoup trauma).3
The retinal opacification can take hours to develop and may involve both the posterior pole and peripheral retina.1,3 The study used animal models to illustrate that the fundus changes represented injury at the level of the photoreceptor outer segments and RPE, which has also been confirmed by histopathological analysis of enucleated human eyes within 24 hours of trauma.3-5 Over the course of up to one week, photoreceptor cells may either recover or undergo degeneration, depending on severity of injury. Photoreceptors that undergo degeneration are then phagocytosed by RPE cells, resulting in secondary RPE migration into the retina.3 Interestingly, animal models have suggested evidence of a transient breach in the blood-retinal barrier in the immediate period following trauma for up to seven days, but this has not been validated clinically.6
Advances in OCT technology allow us to noninvasively image and visualize the retinal tissue response to trauma in vivo at any time interval.1,4,7 Acutely, there is hyperreflectivity and disruption of the photoreceptor inner segment and outer segment (IS-OS) junction and the RPE; chronically, there can be focal IS-OS loss and RPE migration into the retina.4,7 The sequelae related to commotio retinae have been compared with that of photic retinopathy.
While there is no histopathological distinction regarding severity of commotio retinae, there is a clinical description made to distinguish mild vs. severe disease states.1 A milder grayish-white appearance to the retina with presenting VA better than 20/200 is felt to be a retinal concussion, while a more intense whitening of the retina with worse presenting VA is a retinal contusion.7 In either case, commotio retinae is a transient and self-limiting disease with no supported interventional options in the literature.1,4,8 With observation, retinal concussions tend to demonstrate more favorable outcomes, with restoration of vision to, or near, baseline levels; retinal contusions often result in poorer visual outcomes.1,4
At most recent follow-up, the patient’s uncorrected VA measured 20/40 and he is being followed with serial dilated fundus exams with scleral depression. The hyphema resolved without complications, and manifest refraction and gonioscopy are planned for his next visit.
Retina Quiz Answers
1: b, 2: a, 3: d, 4: d, 5: c
Dr. Aboumourad currently practices at Bascom Palmer Eye Institute in Miami. He has no financial disclosures.
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
1. Ryan SJ, Davis JL, Flynn HW, et al. Retina, Fifth ed. London; New York: Saunders/Elsevier, 2013. 2. Berlin R. Zur sogenannten Commotio retinaw. Klin Mbl Augenheilk. 1873;11:42-78. 3. Sipperley JO, Quigley HA, Gass JDM. Traumatic retinopathy in primates: the explanation of commotio retinae. Arch Ophthalmol. 1978;96(12):2267-73. 4. Agarwal A, Gass JDM. Gass’ Atlas of Macular Diseases, Fifth ed. London: Elsevier, 2011. 5. Mansour AM, Green WR, Hogge C. Histopathology of commotio retinae. Retina. 1992;12(1):24-8. 6. Gregor Z, Ryan SJ. Blood-retinal barrier after blunt trauma to the eye. Graefes Arch Clin Exp Ophthalmol. 1982;219(5):205-8. 7. Bradley JL, Shah SP, Manjunath V, et al. Ultra-high-resolution optical coherence tomographic findings in commotio retinae. Arch Ophthalmol. 2011;129(1):107-8. 8. Yanoff M, Duker JS, Ausburger JJ, et al. Ophthalmology, Fourth ed. Philadelphia: Elsevier Saunders, 2014. |

