 |
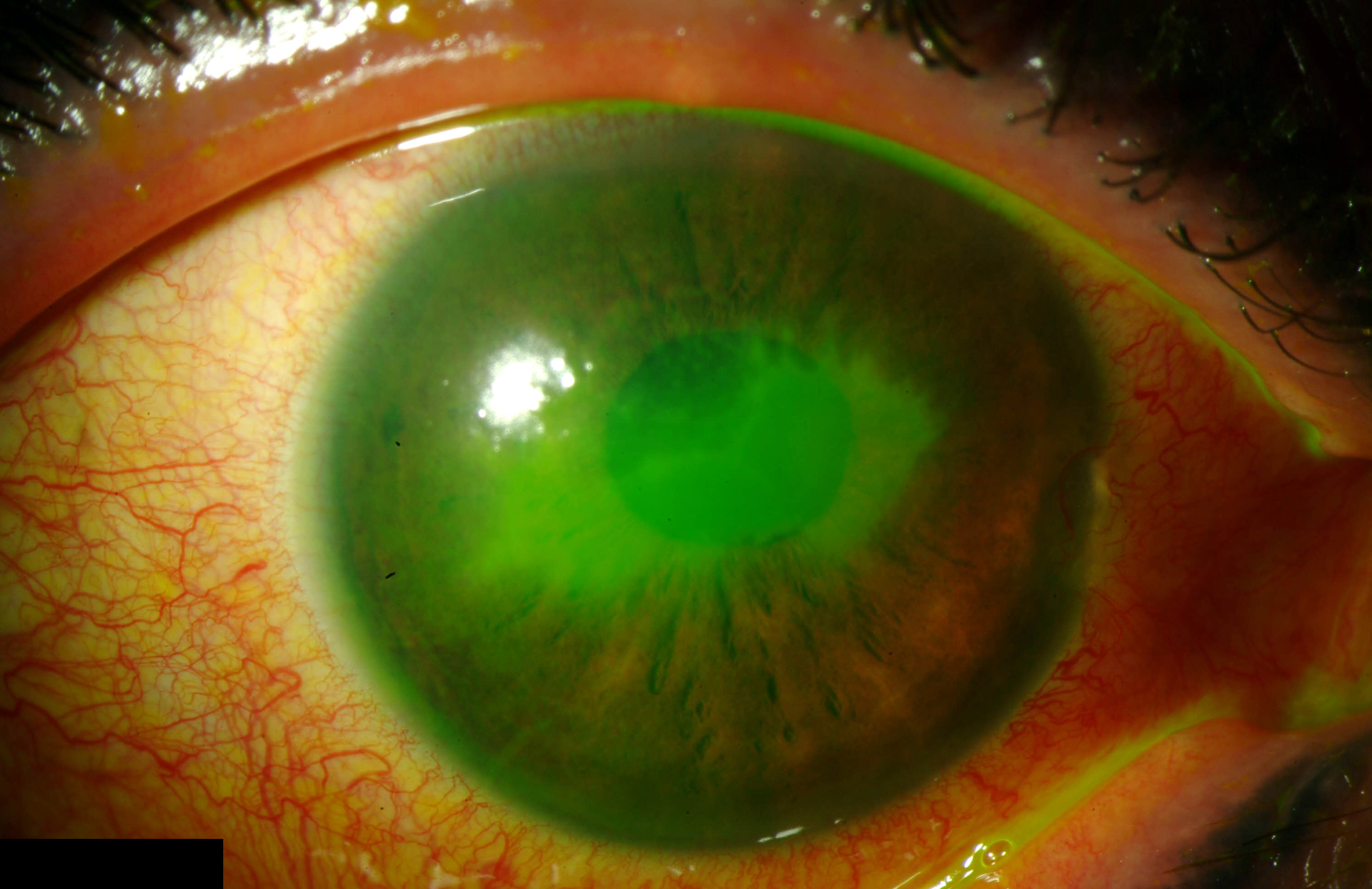
A systemic analysis found a disproportionate underreporting of evidence level in AAOph PPP guidelines over time. Corneal guidelines seemed to fare the worst, with just 5% supported by level I evidence in 2021 vs. 100% in 2012. Photo: Christine Sindt, OD. Click image to enlarge. |
Typically updated every five years, the American Academy of Ophthalmology (AAOph) Preferred Practice Patterns (PPPs) guidelines recommend diagnostic and treatment approaches for various ophthalmic conditions. As medical specialties increasingly rely on evidence-based medicine, researchers recently performed a systematic analysis to evaluate the levels of evidence behind previous and current AAOph guidelines. What they observed was an increasing emphasis on evidence from randomized controlled trials from 2012 to 2021 but an overall decline in the number of practice recommendations with disclosed levels of evidence.
The researchers reviewed all current PPP guidelines and their immediate predecessors from five years prior (applicable for 23 out of 24 current PPPs) with level of evidence recommendations (I [randomized controlled trials], II [case-control or cohort studies] and III [nonanalytic studies]). Level I guidelines are defined by AAOPh as the most important to the patient care process.
They reported in their paper, published in BMC Ophthalmology, that “the number of recommendations with levels of evidence decreased from 1,254 in prior PPPs to 94 in current PPPs.” More specifically, they noted that, “the number of recommendations with level I evidence decreased from 114 to 83, level II decreased from 147 to two and level III decreased from 993 to nine.”
While evidence levels I and II decreased, the proportion of level I recommendations increased from 9% in 2012 to 88% in 2021. A subgroup analysis by subspecialty revealed similar trends (level I recommendations in prior vs. current PPPs: retina: 12% vs. 100%; cornea: 5% vs. 100%; glaucoma: 23% vs. 100%; cataract: 17% vs. 100%). The researchers believe that this increase was primarily driven by a disproportionate underreporting of lower-level evidence.
“On the one hand, this trend suggests guideline authors may have attempted to highlight level I recommendations in the current PPPs,” they emphasized in their paper. “On the other, fully reporting both level I and lower-level evidence could help expand the evidence base highlighted in ophthalmology guidelines.”
“Overall, this study demonstrated that while current guidelines report levels of evidence for substantially fewer recommendations, a much higher proportion of recommendations are supported by evidence from randomized controlled trials,” the researchers wrote in their paper. “While current AAOph PPPs emphasize evidence from randomized controlled trials, the level of evidence from other types of studies may not be formally rated or reported.”
The research team also evaluated whether ophthalmology guidelines included cost/value statements. While 88% did, more than half reported gaps in evidence.
“Cost/value considerations have yet to be incorporated into the development of specific recommendations, representing an avenue for future work in ophthalmology guideline development,” the study authors noted.
Based on this review, the researchers suggest that further AAOph PPP guideline development should explicitly report the level of evidence associated with each recommendation. Additionally, they note that it may be valuable to include cost/value considerations in recommendations.
Song A, Lusk JB, Kuo AN, et al. Systematic analysis of levels of evidence supporting American Academy of Ophthalmology Preferred Practice Pattern guidelines, 2012-2021. BMC Ophthalmol. 2023;23:132. |

