To understand the factors that contribute to AMD further, many researchers have turned their attention toward the gut microbiome. A team based out of the University of Chicago recently explored the association between antibiotic exposure and the development of AMD in epidemiological data. They conducted a large case-control study of a nationwide commercial health insurance claims database that compared antibiotic usage in patients with new-onset AMD to matched controls from the general population. The study demonstrated an association between antibiotic exposure and increased odds of a new-onset ICD code diagnosis of AMD. There also appeared to be a frequency- and duration-dependence to the association, with greater cumulative number of prescriptions and day supply of antibiotics linked with increasing odds.
 |
|
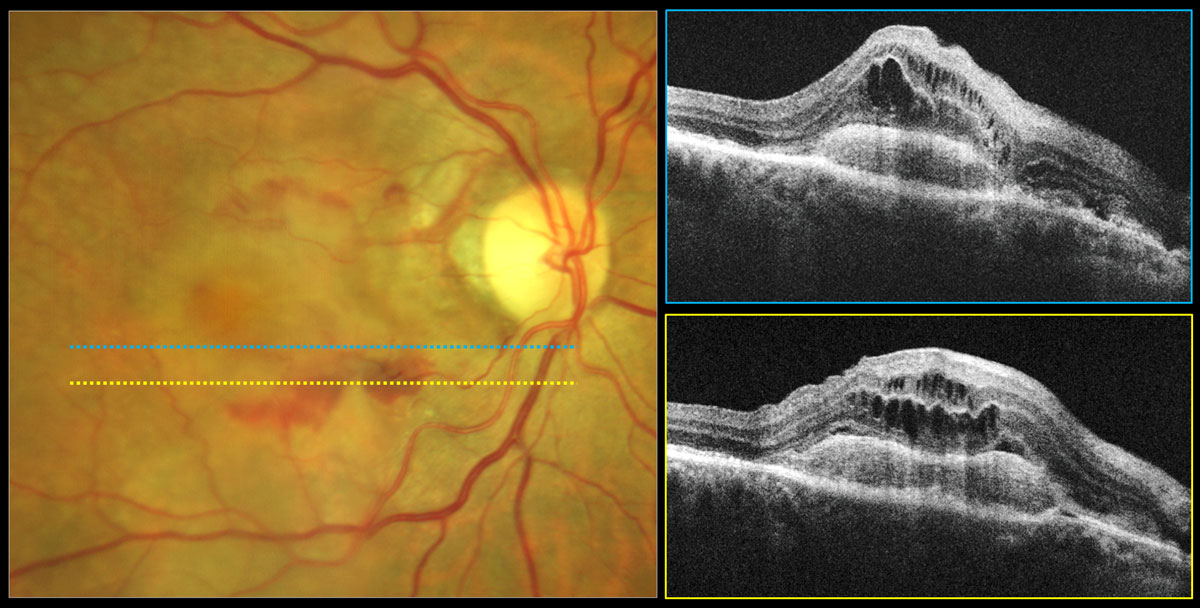
This recent study has suggested that avoiding aminoglycosides and quinolones when an alternative option is available and clinically efficacious should be considered, as it found an increasing odds ratio of diagnosis of wet AMD, but not dry AMD, as the number of prescriptions for these two classes of antibiotics increased. Photo: Carolyn Majcher, OD. Click image to enlarge. |
The nationwide retrospective case-control study analyzed 312,404 cases of patients aged 55 and older with new-onset AMD and 312,376 matched controls from the general population. Exposure to antibiotics in the two years before the index date was determined for cases and controls matched one-to-one by age, year, region, anemia, hypertension and a comorbidity index. The researchers felt that “the older population better captures those at risk of AMD, whereas a 24-month lookback period extends the time that may be required for antibiotics to exert a degenerative effect on the retina.”
Among the antibiotic classes, exposure to aminoglycosides (odds ratio; OR = 1.24) and fluoroquinolones (OR = 1.13) was associated with the greatest odds of a new-onset ICD code diagnosis of AMD. Broad-spectrum antibiotics were associated with nearly three-times greater odds of new-onset AMD (OR = 1.15) compared with narrow-spectrum antibiotics (OR = 1.05).
Notably, fluoroquinolones and aminoglycosides were associated with greater odds of new-onset coding of wet AMD compared to dry AMD.
“These results suggest that fluoroquinolones and aminoglycosides may interact differently with the pathways that drive development and progression of dry and wet AMD,” the researchers wrote in their paper for the IOVS journal. “In support of this, we also found an increasing odds ratio of a new-onset ICD code diagnosis of wet AMD, but not dry AMD, as the number of prescriptions for these two classes of antibiotics increased.”
The study noted that exposure to fluoroquinolones in the six months preceding AMD diagnosis was associated with the greatest odds of a new-onset ICD code diagnosis of AMD compared with exposure at six to 12 months or one to two years. The researchers believed that this data may support the notion that fluoroquinolones mediate an acute inflammatory or cytotoxic effect that accelerates AMD development in patients with a heightened baseline risk.
“Although it is too early to draw definitive conclusions and to substantially alter clinical practice due to these findings, several results merit consideration,” the researchers wrote in their paper. “Our results suggest that use of fewer prescriptions, limiting total days of exposure and choosing agents with appropriately narrow coverage may be important components of antibiotic stewardship to prevent AMD development.”
Moir J, Hyman M, Wang J, et al. The association of antibiotic use and the odds of a new-onset ICD code diagnosis of age-related macular degeneration: a large national case-control study. Invest Ophthalmol Vis Sci. 2023;64(12):14. |

