 |
A 64-year-old black female presented complaining of difficulty reading and occasional redness. She denied having pain or discomfort and has never worn glasses or had an eye exam. During the history, the patient noted that the right side of her body has been weak for about three years. She uses a cane to help her walk.
Best-corrected visual acuity was 20/20- O.U. Confrontation fields were full to careful finger counting O.U. Extraocular motility was full, with no pain or diplopia on eye movement. Pupils were equally round and reactive, without an afferent pupillary defect. IOP measured 14mm Hg O.U. Anterior segment exam was unremarkable.
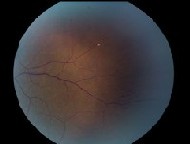
Dilated fundus exam of the left eye was significant for the changes shown in figures 1 and 2. The right eye was completely normal.
 |
| 1. A montage photo shows the posterior pole O.S. and extends to the peripheral retina. |
 |
| 2. A magnified view of the temporal retina shows suspicious areas. |
Take the Retina Quiz
1. What do the white spots in the fundus photograph represent?
a. Talc retinopathy.
b. Hollenhorst plaque.
c. Biettis crystalline dystrophy.
d. Peripheral drusen.
2. What additional information in this patients history will likely be positive?
a. Transient ischemic attacks.
b. Night vision problems.
c. Amaurosis fugax.
d. Both a and c.
3. What additional testing would be most useful for this patient?
a. Tensilon test.
b. Carotid Doppler ultrasonography.
c. Gonioscopy.
d. Optical coherence tomography.
4. What is the correct diagnosis?
a. Branch retinal artery occlusion.
b. Ocular ischemic syndrome.
c. Talc retinopathy.
d. Bacterial endocarditis.
5. What complaint do patients often report with this condition?
a. Eye pain.
b. Light sensitivity.
c. Metamorphopsia.
d. Intermittent diplopia.
6. What would be the appropriate management for this patient?
a. IOP-lowering medications.
b. Referral for cardiology work-up and possible endarterectomy.
c. Panretinal photocoagulation.
d. All of the above.
For answers, go to bottom of page.
Discussion
The fundus photos of our patient show several small glistening, refractile plaques at bifurcations of the retinal arteries. These are Hollenhorst plaques, microemboli that likely originate from larger plaques, usually in the carotid arteries. She also has multiple blot hemorrhages that extend almost 270 degrees in the peripheral retina.
 |
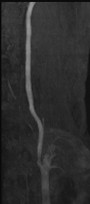 |
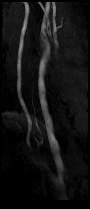
| 3, 4. Magnetic resonance angiography of the carotid arteries (O.D. left, O.S. right). Shows a difference between the two. |
TIAs represent a temporary loss of motor and/or sensory function due to a disturbance in the blood supply to the brain. Considered mini-strokes, TIAs usually occur when emboli become dislodged from the heart or carotid arteries or due to severe carotid artery stenosis. Patients who have TIAs may experience weakness and/or numbness in parts of the body, particularly on one side, and may experience double vision and trouble with speech.
When TIAs are embolic, symptoms become apparent when the dislodged plaques block the blood flow as the embolism travels in the blood stream to the various parts of the brain. Symptoms may be fleeting or temporary as the plaque moves forward through the brain.
More importantly, the symptoms are a harbinger of an impending stroke. About 10% of patients suffer a stroke within 90 days of a TIA.1 Other studies show that one out of three people suffers a stroke within a year of a TIA.2 So, patients whose symptoms are consistent with TIAs should be sent for emergency work-up of their carotid arteries.
Amaurosis fugax occurs due to retinal TIAs. Patients may experience painless, monocular episodes in which their vision dims or completely blacks out. These episodes can last from several seconds to hours as the plaques pass through the retinal circulation. Once passed, vision will return to normal. A larger plaque can completely block the circulation, resulting in a branch or central retinal artery occlusion.
Ask if the patient is experiencing any TIA-like symptoms or amaurosis fugax. Any symptoms warrant a medical work-up that pays particular attention to the heart and carotid arteries and includes a lipid profile. Carotid duplex ultrasonography is a reliable noninvasive imaging test. Magnetic resonance angiography (MRA) with contrast can also help evaluate the cerebral and cervical vessels.
When patients have retinal artery plaques but no symptoms, you should still evaluate the source of the plaque.3 Doing so may prevent a devastating visual event or stroke.
Our patient presented with several obvious Hollenhorst plaques. She also had a peripheral retinal hemorrhage that we have yet to address. Upon further questioning, she said that she had a left-sided stroke in 2000 and underwent endarterectomy on the right side. This explains why our patient walks with a cane.
Further work-up of her carotid arteries revealed good graft placement on the right side and nearly 100% flow of the internal and external carotid arteries. MRA, however, revealed approximately 85% blockage of the left internal carotid artery. Our patient evidently suffers from ocular ischemic syndrome (OIS) in her left eye as well.
OIS has various presentations that primarily relate to a lack of perfusion pressure to the eye. It primarily affects patients as they near age 65. Bilateral involvement occurs in 20% of patients and generally results in 90% stenosis of the ipsilateral carotid arterial system.4 This amount of blockage is sufficient to reduce ocular perfusion pressure by about half and to present clinically as central retinal artery pulsation.4
Patients who have OIS may present with a slow onset of vision loss and may complain of a dull ache around their eye or experience amaurosis fugax. About two-thirds have iris rubeosis and either elevated IOP from angle neovascularization or decreased IOP/hypotony from ciliary body ischemia.4 Anterior chamber flare and corneal edema may be seen. Midperipheral retinal hemorrhages, dilation and tortuosity of the retinal veins, and a pulsating retinal artery also are hallmarks.
Our patient had a reasonably good outcome following her initial endarterectomy on the right side. The vascular surgeons have deferred surgery on the left side, as they believe she has reasonably good collateral circulation.
We prescribed reading glasses to address her visual complaints. We suspected that the redness she complained about was due to dry eyes, so we recommended using artificial tears at least t.i.d. or q.i.d.
We continue to monitor her for complications related to her OIS and retinal plaques and encourage her to comply with her primary-care physicians instructions.
This case was co-authored by Paul E. Collins, O.D., an optometric resident at Bascom Palmer Eye Institute in Miami.
1. Johnston SC. Clinical practice. Transient ischemic attack. N Engl J Med 2002 Nov 21;347(21):1687-92.
2. MedlinePlus Medical Encyclopedia, Transient ischemic attack (TIA). www.nlm.nih.gov/medlineplus/ency/article/ 000730.htm. Accessed December 15, 2005.
3. Hayreh SS. Prevalent misconceptions about acute retinal vascular occlusive disorders. Prog Retin Eye Res 2005 Jul;24(4):493-519.
4. Sharma J, Brown GC. Ocular Ischemia Syndrome. In: Ryan SJ, Schachat AP, Murphy RP, eds. Retina, Vol. IIMedical Retina. 3rd ed. St. Louis: Mosby-Year Book, 2000:1516-29.
Answers: 1)b; 2)d; 3)b; 4)b; 5)a; 6)b.

