 |
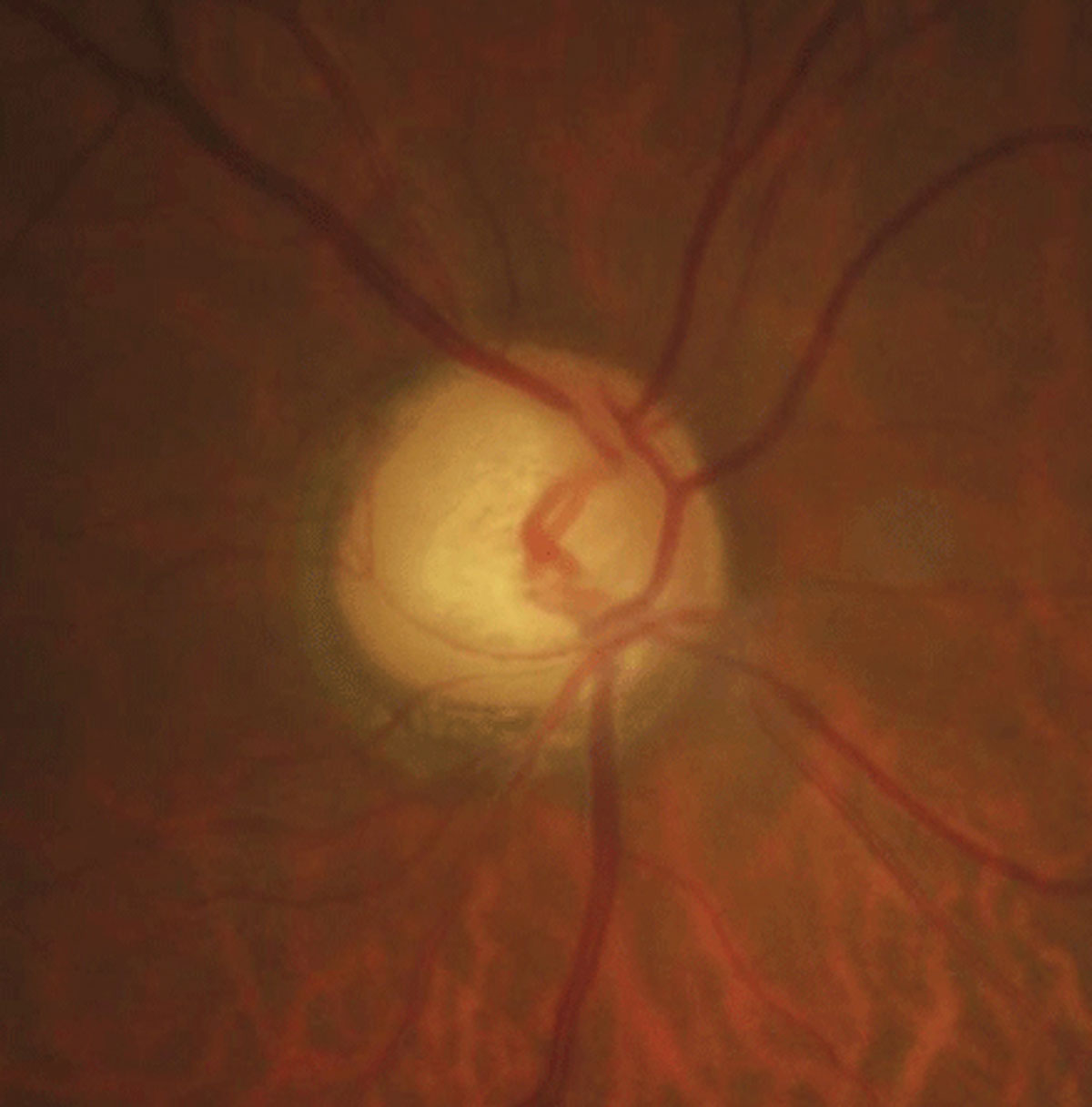
| The study found that Latinos have a higher disease prevalence than Chinese Americans, yet this difference is not as significant due to the latter group’s higher myopia prevalence. Photo: Justin Cole, OD, and Jarett Mazzarella, OD. Click image to enlarge. |
Researchers recently examined data from two population-based studies to assess whether the roles of certain primary open-angle glaucoma (POAG) risk factors—specifically refractive error and ocular biometrics—may differ between Latino and Chinese Americans. They observed that the POAG risk conferred by myopic refractive error and longer axial length was similar in both populations, though the unadjusted disease risk was 1.6-times higher among Latinos. However, “the difference in POAG prevalence between the two groups is narrowed by higher myopia prevalence among Chinese Americans,” the researchers concluded in their paper on the study.
Data from both the Los Angeles Latino Eye Study (LALES) and the Chinese American Eye Study (CHES) was included in the retrospective analysis, totaling 7,601 phakic participants (47.3% LALES, 52.7% CHES). All were at least 50 years old, with the mean age approaching 61 years, and 60.9% of participants identifying as female.
The analysis revealed a higher prevalence and unadjusted risk of POAG in LALES than CHES (6.0% and 4.0%, respectively; odds ratio [OR]: 1.55). In the multivariate analysis, the researchers reported the most significant risk factors for POAG to be Latino ethnicity (OR: 2.25), refractive myopia (OR: 1.54 for mild, OR: 2.47 for moderate, OR: 3.94 for high compared with non-myopes) and longer axial length (OR: 1.37 per 1mm).
“Axial length was 2.7-fold more strongly associated with POAG than high myopia status,” the researchers wrote in their paper. Notably, they determined that “there was no modifying effect by race/ethnicity on the association between refractive error (per diopter) or axial length (per millimeter) and POAG.”
The researchers noted that no specific factors have yet been strongly linked to the higher prevalence of POAG among Latinos, and the data presented in this study doesn’t help to make sense of the discrepancy, either. “These findings demonstrate that the difference in POAG prevalence between Latino and Chinese Americans is narrowed by the higher prevalence of refractive and axial myopia among Chinese Americans; however, they do not explain why the adjusted risk of POAG is also higher in LALES,” they wrote. What the findings do suggest is that the higher POAG risk in Latino Americans is not related to myopic refractive error or longer axial length.
The study authors concluded their paper by stating that there is a need for further study of other factors that may contribute to the higher POAG risk in Latinos and potentially other races/ethnicities. They also argue that “racial/ethnic populations [such as Chinese Americans] with higher myopia incidence may become disproportionately affected by POAG in the context of the global myopia epidemic.”
Zhou S, Burkemper B, Pardeshi AA, et al. Racial and ethnic differences in the roles of myopia and ocular biometrics as risk factors for primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 2023;64(7):4. |

