 |
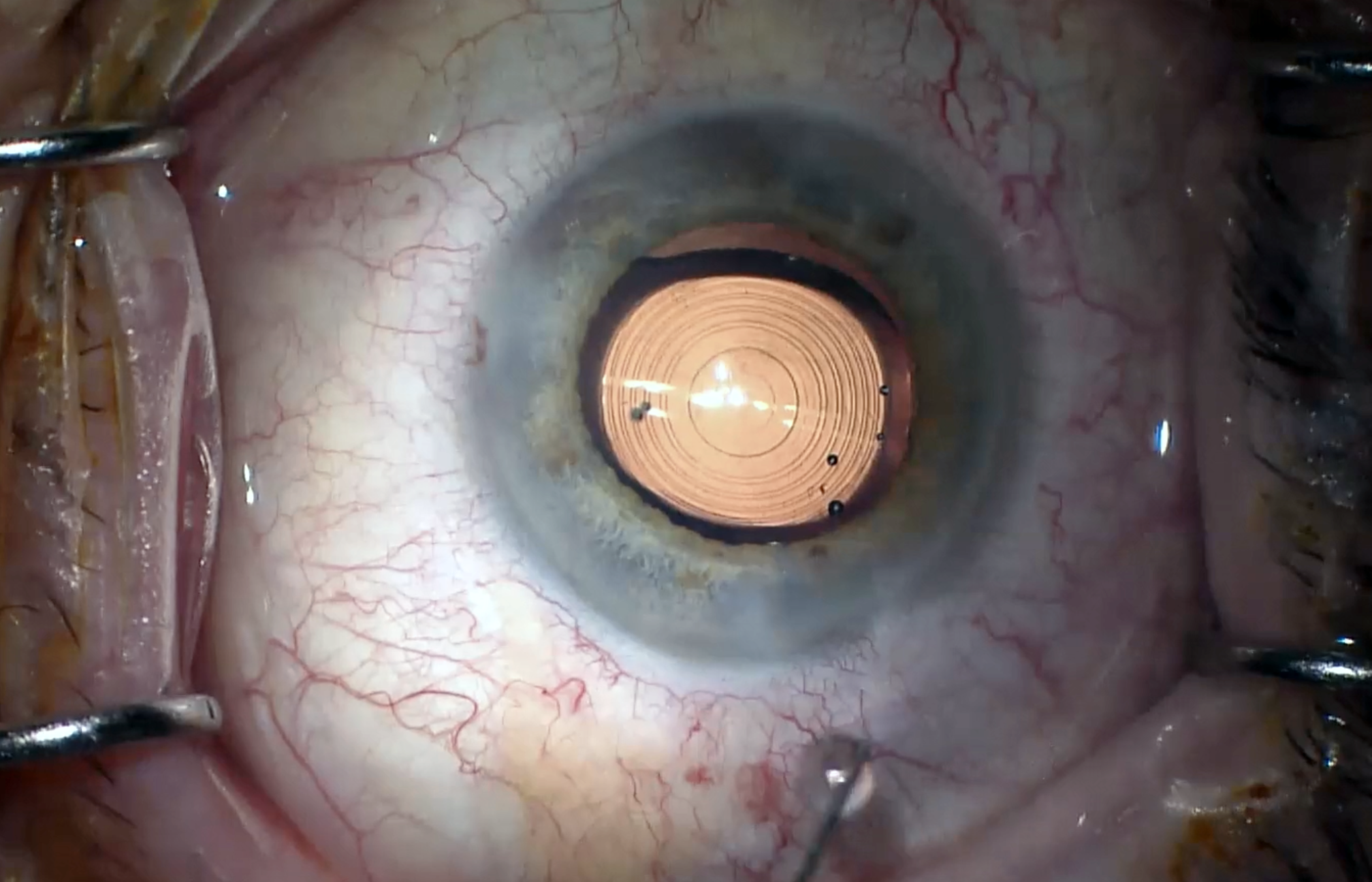
| Pseudophakic patients with AMD or ERM showed similar contrast adaptation as healthy controls in this study. Photo: Ethan Zimmerman, OD. Click image to enlarge. |
A recent study was conducted to determine whether contrast adaptation is compromised in pseudophakic patients with macular disorders such as age-related macular degeneration (AMD) or epiretinal membranes (ERM), as this could have implications for the tolerability of presbyopia-correcting intraocular lenses (IOLs). Its data demonstrated that these conditions have no effect on the visual system’s adaptation to low-contrast or blurred retinal images, and therefore, the researchers argue that macular disorders don’t belong on the list of strict exclusion criteria for presbyopic IOL implantation.
Included in the study was a small cohort of 10 patients with dry mild to moderate AMD or ERM, all of whom had been implanted with a monofocal IOL (Asphina 409, Zeiss) and showed metamorphopsias during Amsler test evaluation. These patients, in addition to 10 healthy controls, were tested to quantify contrast adaption after +4.00D defocus for 10 minutes, by performing an interocular contrast matching task, which the researchers described in their paper for Current Eye Research: “Subjects manually adjusted the perceived contrast of the test patch as seen by the test eye to match to the contrast of a target patch with a fixed Michelson contrast of 0.2 as seen by the contralateral untreated eye.”
The team reported that patients with AMD or ERM subjectively matched the 0.2 target contrast with a contrast of 0.24 before adaptation and 0.19 after adaptation, equating to an induced contrast gain by adaptation of 0.05 (27%). This value was not significantly different from the control group, which showed an induced contrast gain by adaptation of 0.06 (35%).
“The results presented here allow us to consider that also the visual system of patients with mild to moderate macular disorders can compensate for the optical limitations imposed by presbyopia-correcting IOLs as well as it does in subjects with healthy retinae,” the researchers noted in their paper. “Thus, the presence of a mild to moderate macular disorder (AMD or ERM) should not be prejudicial to the selection of a presbyopia-correcting IOL in cataract surgery,” they advised.
Since macular disease such as AMD can lead to progressive loss of visual function, the study authors suggested that “modern extended depth-of-focus IOLs seem to be the best compromise for patients with macular disorders, as the induced decrease in contrast sensitivity is low, but the patient still benefits from good far and intermediary vision.” If a trifocal IOL is being considered, virtual IOL simulation technology may allow for the assessment of visual performance without having to implant the lens, the researchers pointed out.
While the presence of a macular disorder didn't appear in this study to affect contrast adaptation in patients with monofocal IOLs, the study authors reiterate the numerous other factors there are to consider, such as residual refractive error, dry eye and age.
Kaymak H, Neller K, Graff B, et al. Contrast adaptation in pseudophakic patients with macular disorders. Curr Eye Res. 2024; 49:2, 207-213, |

