 |
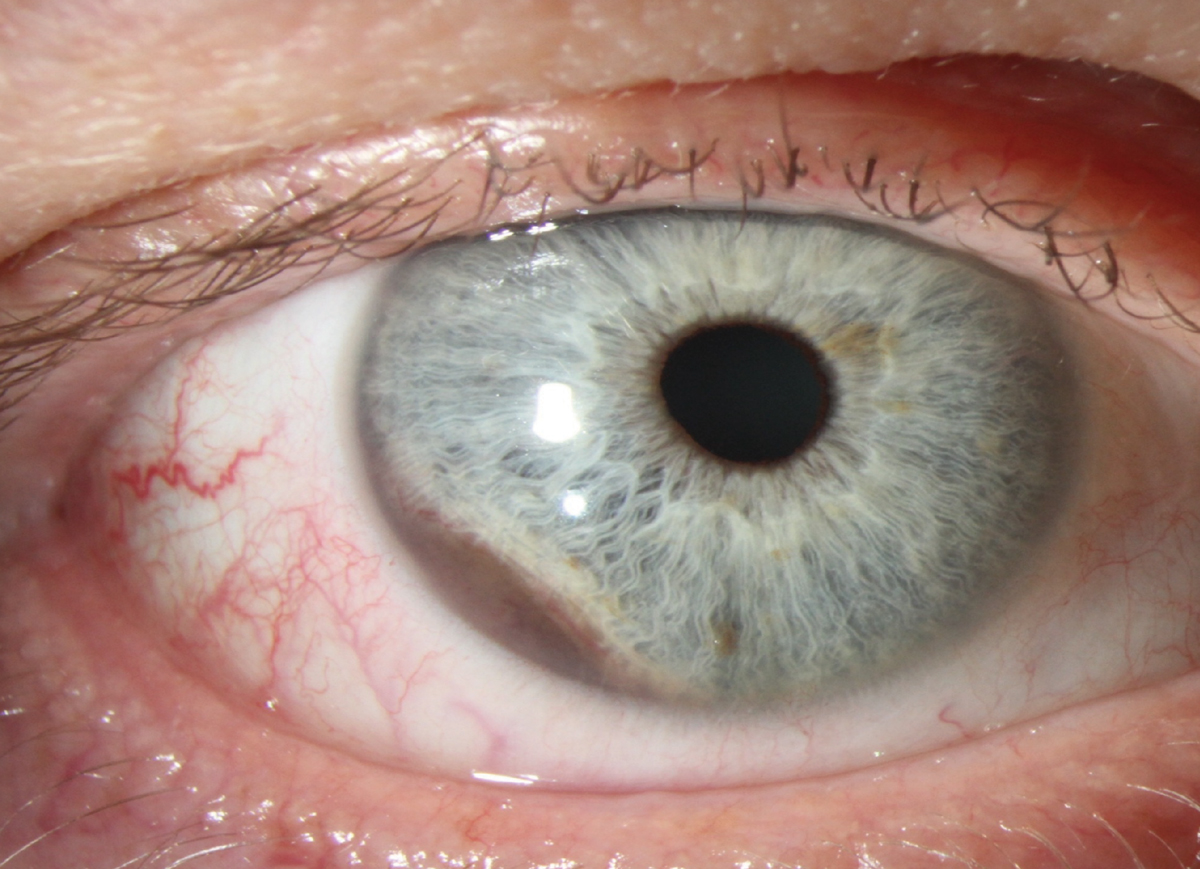
Many eye clinicians go through their entire career without ever seeing the ciliary body. Most ophthalmic records do not even list the ciliary body as a structure to be assessed. If a malignant melanoma there spreads anteriorly to the iris, it is easier to detect in a blue-eyed patient. The obvious iris lesion in Figure 1 would be difficult to detect if the patient had dark brown eyes. Eye color may have been the factor in detection and successful treatment. Early detection and intervention are crucial to increase the odds of patient survival.
Case
A 60-year-old Caucasian woman, who was a long-term patient in our private practice (JS), presented for a routine follow-up. The patient had no symptoms and reported excellent vision in both eyes after routine cataract extraction with posterior chamber IOLs several years earlier. She mentioned that her daughter occasionally observed redness in her right eye but only when her mom looked to the left. The external exam was unremarkable, except biomicroscopy that revealed possible sentinel vessels temporal to the limbus in the right eye at eight o’clock. A small, corresponding iris abnormality was noted in this brown-eyed patient.
 |
|
Fig. 1. A different patient than the case presented; note the blue eyes. A ciliary body malignant melanoma is invading the iris from seven to nine o’clock OD. Possible sentinel vessels at nine o’clock secondary to a ciliary body malignant melanoma below. Could this lesion be missed if this patient had dark brown eyes? Click image to enlarge. |
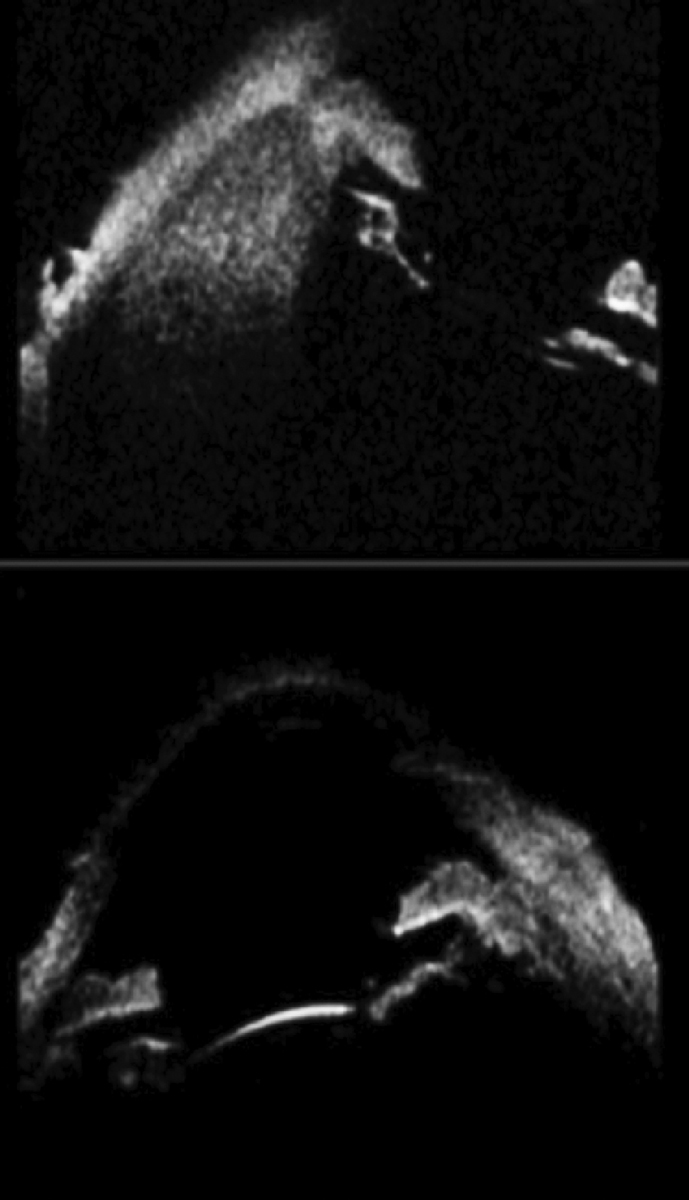
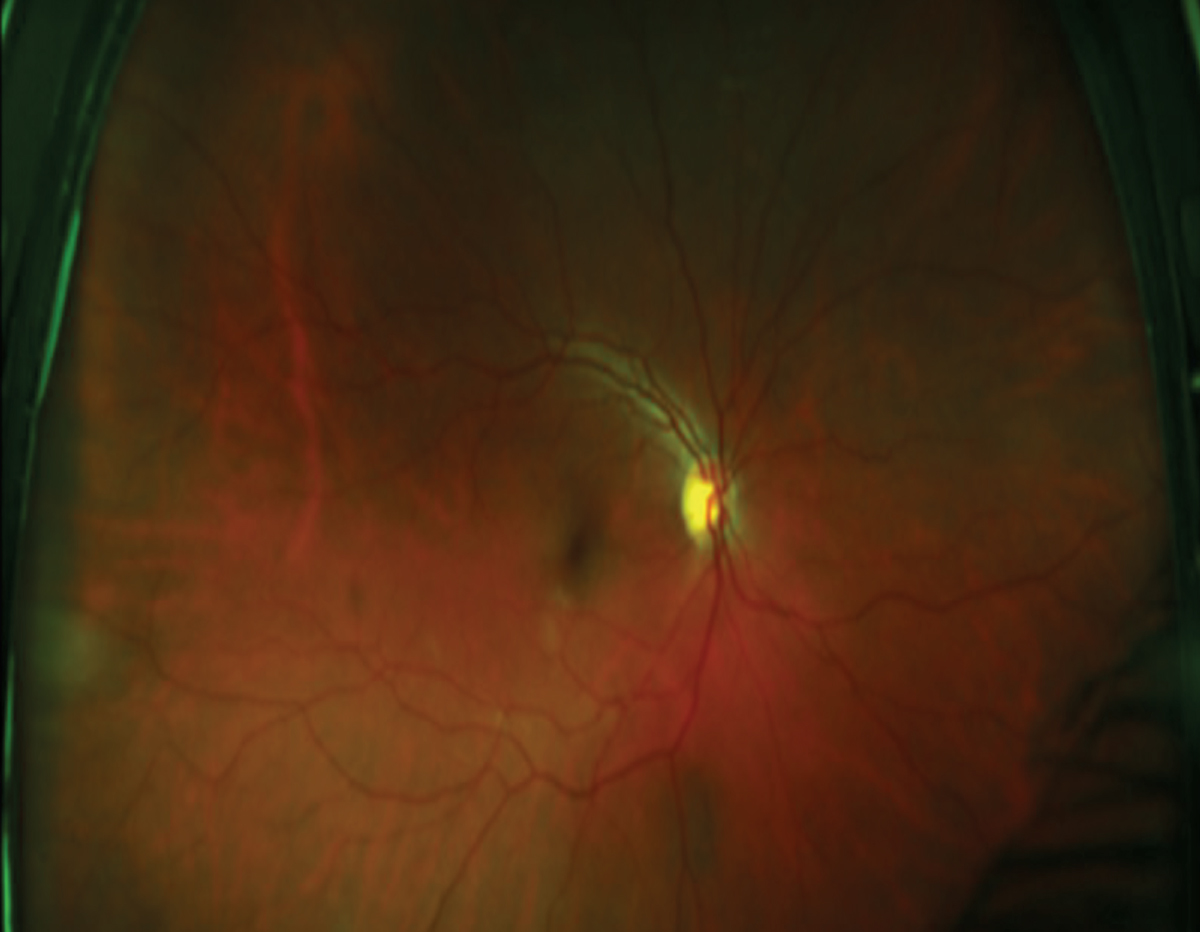
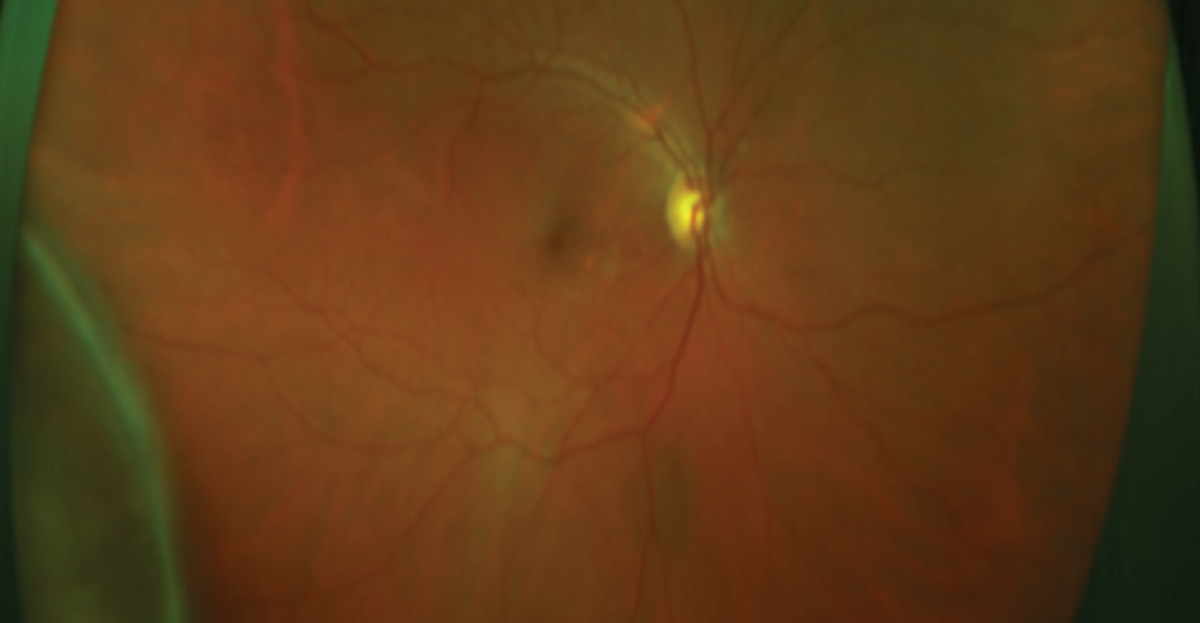
This practice had an ultrasound biomicroscopy (UBM) device. Immediate scans demonstrated a mass lesion of the ciliary body at eight o’clock (Figure 2). After dilation, ultrawidefield Optos images with and without steering revealed a dark peripheral lesion in the right eye between seven and nine o’clock. A review of previous images about a year earlier without steering revealed a possible smaller lesion in the temporal periphery at nine o’clock in the same eye (Figures 3 and 4).
The patient was immediately referred to David Abramson, MD, chief of ophthalmic oncology at Memorial Sloan Kettering in Manhattan, who confirmed the diagnosis of a ciliary body malignant melanoma extending posteriorly to the choroid. The patient was then treated with iodine plaque (I-125). The lesion regressed over the next six months, with a PET scan failing to reveal metastasis.
You Be the Judge
If the patient had blue eyes instead, could the detection of the melanoma have been made a year earlier?
Assuming the patient had blue eyes and not dark brown ones, could a “FAT scan” (see below) performed after the actual diagnosis support successful malpractice litigation?
Since the patient was under post-op care for bilateral cataract removal and presbyopia-correcting IOLs in the same practice, should the malignant melanoma have been discovered earlier, and hence the prognosis would have been improved?
Is steering with ultrawidefield imaging the standard of care?
If steering was performed a year earlier, could the treatment have commenced a year earlier?
 |
|
Fig. 2. Two UBM sections of the anterior segment. At eight o’clock (top image) is the ciliary body malignant melanoma. The section through 10 and four o’clock (bottom image) does not reveal any gross abnormality. Click image to enlarge. |
Our Opinion
A “family album tomography” (FAT) scan—careful review of pictures of a patient’s face—may sometimes reveal a finding missed by the clinicians providing care to the patient. If our patient had blue eyes and if an iPhone picture of the patient’s face was taken earlier, zoomed in and revealed a brown spot on the iris, the plaintiff’s attorney and experts could argue that the melanoma had already spread to the iris earlier and was missed during a routine exam.
Steering is considered useful to obtain images of the far peripheral fundus. One could argue whether doing that a year earlier would have detected the melanoma. We recommend steering in the vast majority of cases, but it is unclear whether it is the standard of care right now with ultrawidefield imaging. Binocular indirect ophthalmoscopy is the standard of care and should include steering whenever possible.
 |
|
Fig. 3. Optos ultrawidefield image OD about a year prior to the diagnosis. Is the subtle peripheral dark zone between between eight and 10 o’clock normal or an early choroidal melanoma? Click image to enlarge. |
Follow-Up
The patient was lost to follow-up, and malpractice litigation was initiated but never completed. An attempt is presently underway to investigate the outcome of this case further from Memorial Sloan-Kettering Cancer Center.
UBM
Only a minority of ophthalmic clinicians have access to this imaging system, and it is often never performed routinely. However, UBM is considered to be ideal in viewing the ciliary body. Structures that are opaque to light can often be visualized with sound. With UBM, the differential diagnosis of a cystic vs. a solid lesion is straightforward in a majority of cases.1
B-scan ultrasound is generally not helpful in detecting tumors of the ciliary body, the exception being that if the tumor has spread posteriorly to the choroid and has enlarged considerably. B-scan ultrasound is most useful to detect abnormalities in the posterior segment such as retinal detachments and mass lesions in the orbit. UBM has far better resolution of the anterior segment than B-scan but does not penetrate well. Hence, that is the trade-off, and one technology does not replace the other.
 |
|
Fig 4. The lesion between seven and nine o’clock is a choroidal melanoma, which is the posterior extension of the ciliary body malignant melanoma. Click image to enlarge. |
When to Consider UBM
When a brown spot is visualized at the far peripheral iris, especially one that was not documented previously.
When the angle appears to be narrower in one or several clock hours than in the remaining hours, and gonioscopy fails to reveal its cause.
When there is localized perilimbal redness in one zone and in one eye only. Is this evidence of a so-called “sentinel” vessel suggestive of a lesion below?
Finding Uveal Melanomas
These are considered as the most common malignancy of the eye in Caucasian adults and rare, but occasionally encountered, in Black and African American adults. In the Caucasian population, there are approximately four to eight new cases per year per million population. A malignant melanoma can begin in any of the three components of the uveal tract, but only about one in 10 begin within the ciliary body.2
An isolated malignant melanoma of the iris is considered to have the most favorable prognosis, and one of the ciliary body and anterior choroid has the worst. The 10-year mortality rate of ciliary body malignant melanoma reaches 30% to 50%. Knowing that the shortest average doubling time of primary uveal melanoma is 154 days, ophthalmic oncologists can calculate the size of the tumor at any previous eye exam.3
This information is sometimes used in malpractice cases to prove or disprove that the tumor was detectable. In such cases, the reference is “a like practitioner under like circumstances” and not the specialists at facilities such as Memorial Sloan Kettering.
Of note, Julia Canestraro, OD, is a graduate of SUNY Optometry who is presently at Memorial Sloan Kettering in the Ophthalmic Oncology Service and is helpful in coordinating referrals and follow-ups.
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Bass is a Distinguished Teaching Professor at the SUNY College of Optometry and is an attending in the Retina Clinic of the University Eye Center. She has served as an expert witness in a significant number of malpractice cases, the majority in support of the defendant. She serves as a consultant for ProQR Therapeutics.
1. Turner ML, de Alba Campomanes AG, Stewart JM, Oatts JT. Congenital ciliary body cysts causing lens abnormalities and secondary angle closure glaucoma in a child. Am J Ophthalmol Case Rep. 2022;28:101723. 2. Costache M, Patrascu OM, Adrian D, et al. Ciliary body melanoma—a particularly rare type of ocular tumor. Case report and general considerations. Maedica (Bucur). 2013;8(4):360-4. 3.Singh AD. Uveal melanoma: implications of tumor doubling time. Ophthalmology. 2001;108(5):829-30. |

