 |
The American Optometric Association–sponsored InfantSee Program has been quite successful and resulted in an increase in the number of infants between six and 12 months old evaluated by optometrists. These free exams have uncovered myriad disorders including strabismus, high refractive errors, amblyopia and occasionally pathologies, such as cataracts, congenital toxoplasmosis and optic nerve hypoplasia.
It is crucial to recognize that changes in refractive error over the first few years of life may indicate a serious pathology such as an orbital or retinal tumor.
Case
Amanda was first examined by eye care practitioner (Dr. J) at seven months of age for an InfantSee exam. Her mom reported nothing unusual but heard about the free exam and thought it would be a good idea to have her youngest examined. The evaluation was rather routine, and all findings, including a dilated fundus exam (DFE) with binocular indirect ophthalmoscopy, were assessed as within normal limits. The measured refractive error was +1.50D OD and + 1.00D OS. The mom was reassured that all was okay and that glasses for the minor refractive error were not necessary now.
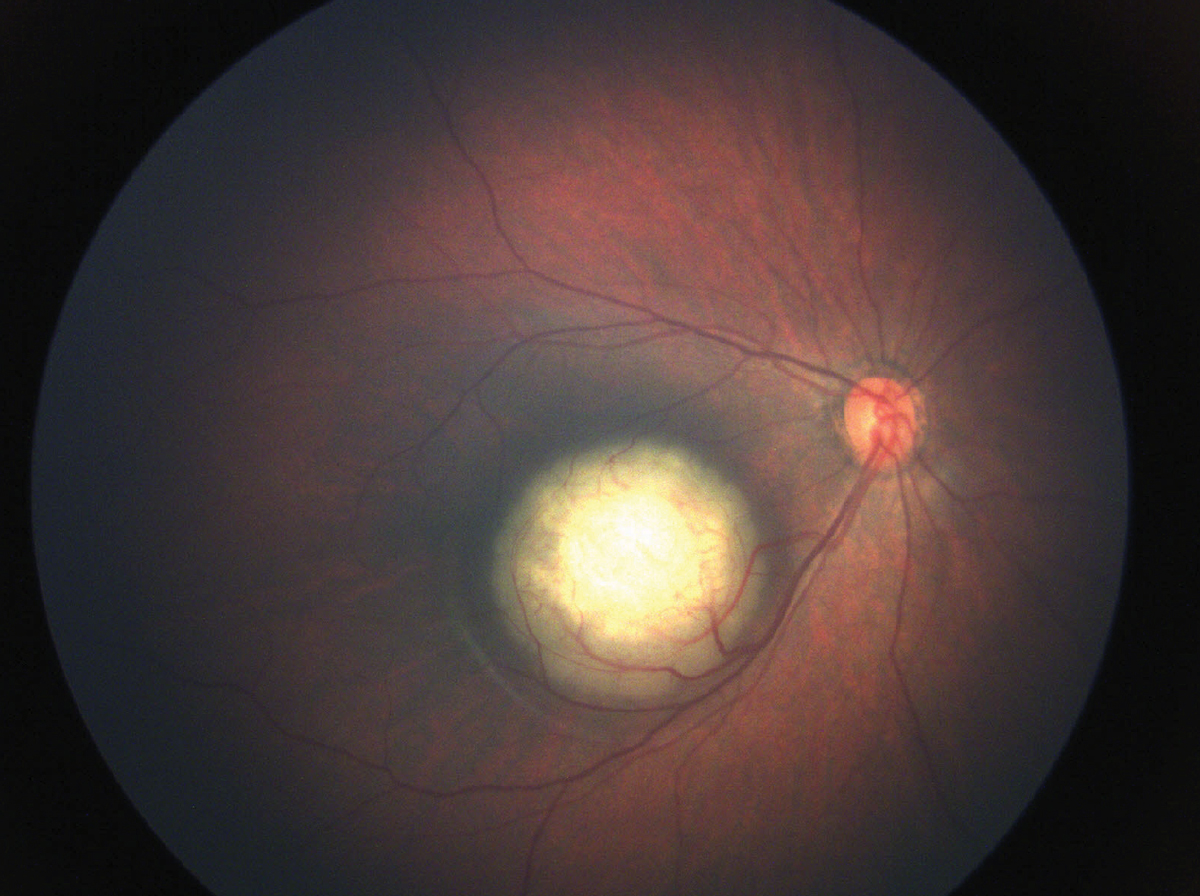 |
| Right eye from a different patient with a retinoblastoma within the arcades and impinging on the fovea. Since the lesion includes the fovea, the axial length will decrease and the refractive error will become more hyperopic. Like the case in question, there was no retinoblastoma in the fellow eye and hence, the anisometropia will increase. Photo: Julia Canestraro, OD. Click image to enlarge. |
As recommended, the mom made an appointment a few months later before Amanda’s first birthday. Again, no symptoms were reported and the exam, including a DFE, was noted as normal. The optic disc, macula, vessels and mid and far peripheral retina were judged by Dr. J as normal. The refractive error on this exam was + 3.50D OD and +1.50D OS. Both exams were performed under the same cycloplegic conditions. The mom was reassured and correction of the refractive error was discussed but not highly recommended. The OD scheduled a follow-up appointment in one year. The mom did not keep the appointment, perhaps because she recognized this exam would not be a “freebie.”
About 18 months later, mom noticed what she thought was an occasional white spot in her daughter’s right pupil. More recently, the dad took iPhone pictures of all four kids together and noticed that only Amanda appeared to have slightly different colored pupils. On a routine scheduled exam two weeks later, the mom mentioned it to her daughter’s pediatrician. The pediatrician attempted to do an external and internal eye exam on this now fidgety, nearly three-year-old but with minimal success. He strongly recommended an exam by a new pediatric ophthalmologist in town who was very good with kids and quite thorough.
About a month before her third birthday, Amanda was examined by the pediatric ophthalmologist who was highly recommended by her pediatrician. This young and highly trained physician immediately noted the hint of a white pupil in the right eye in several positions of gaze. The DFE revealed a white mass in the macula of the right eye extending to the temporal retina. B-scan ultrasound confirmed a mass retinal lesion OD, which matched the observations made with the DFE. The fellow left eye was judged to be normal with both DFE and B-scan ultrasonography.
The pediatric ophthalmologist and several subsequent ophthalmic oncologists all agreed with the diagnosis of retinoblastoma in the right eye only.
You Be the Judge
- Should the optometrist who performed the two InfantSee exams have realized that the change in refractive error may have been a sentinel sign of an underlying problem?
- Are increases in hyperopia as common in infants as increases in myopia?
- Should the optometrist have known that anisometropia followed by a further increase in anisometropia in infants are both quite unusual and an indication of a potential problem?
- Would a like practitioner under like circumstances have provided the same level of care as this optometrist?
- Since the OD did not charge a fee for the two exams, do you agree that he cannot be held culpable of malpractice?
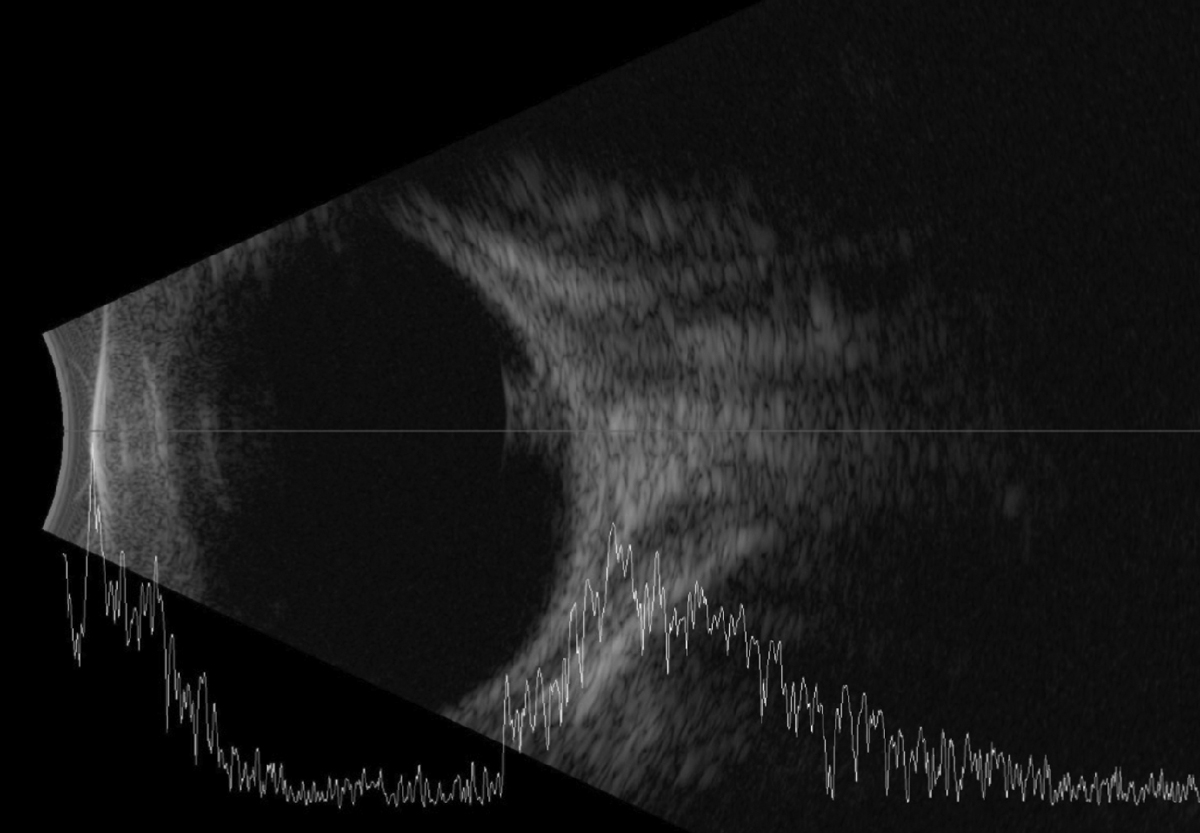 |
| The B-scan reveals a mass in the posterior pole and close to the optic nerve head. Photo: Julia Canestraro, OD. Click image to enlarge. |
Comments and Our Opinion
There are two refractive error clues that often go unrecognized by many clinicians but may suggest a possible retinal, choroidal or orbital mass. The first is increasing hyperopia in the first several years of life, which contradicts the anticipated decrease in hyperopia expected in most normal infants.1 Increases in myopia, in contrast, are somewhat more common. Even a small retinoblastoma in the macula will decrease the axial length and hence increase hyperopia. It has been reported that a 1mm change in axial length can alter the refractive error by 2.50D to 3.00D.2 The vast majority of ODs rarely measure axial length in infants, but most of us do perform retinoscopy on almost every exam.
In a recent study of more than 12,000 newborns, researchers concluded that “anisometropia is present in a very limited number of cases, reported as 0.01%.”3 Knowledge of this study may prove to be vital in select cases to prevent blindness and perhaps death.
Anisometropia in an infant followed by a further increase in anisometropia six months later would be most applicable to unilateral or bilateral (but asymmetric) retinoblastoma. An orbital tumor compressing the posterior pole of the globe can also result in anisometropia.
In this case, the hyperopia increased by 2.00D OD and 0.50D OS and the anisometropia increased from 0.50D to 2.00D.
Would a like practitioner under like circumstances recognize these changes as a red flag? Unsure, I (JS) very recently decided to ask my new associate, Diana Geraghty, OD, (who graduated from SUNY Optometry in June 2023, as the #1 in her class of nearly 100) about these findings. Dr. G thought for a moment, and then this humble superstar responded that, with a normal DFE, she would have attributed these refractive error findings to her less-than-perfect retinoscopy. Of course, we will never know in this case whether the retinoblastoma OD was or was not visible with a routine DFE with binocular indirect ophthalmoscopy.
In many cases of alleged malpractice, most reasonable clinicians and experts can agree when the care rendered clearly deviated from the acceptable standard. In this unfortunate case, it is far more difficult to conclude culpability, or lack thereof.
Most legal and health experts will argue that it matters little or none at all if the exam was performed as a “freebie.” Once a doctor enters into a patient/doctor relationship, the doctor has the responsibility to provide care at the existing standard, regardless of the fee. However, if such a case goes to trial, a jury member may take that into account and have sympathy for the doctor. In a minority of states, a unanimous verdict is required for civil cases, such as malpractice allegations.
Follow-up
Amanda was taken by her parents from specialist to specialist in surrounding states. The final decision was to enucleate the right eye. The left eye remains tumor free. Amanda can wear her prosthetic eye successfully but on rare occasions it dislodges at school, and she is then quite embarrassed.
Not surprisingly, a lawsuit was filed based upon the premise that a diagnosis two or so years earlier could have resulted in successful treatment without sacrificing the eye. Numerous experts gave depositions via Zoom with contradictory opinions. Prior to a jury trial, the case was settled for an amount alleged to be shy of a million dollars. We wish Amanda, her family and the optometrist the best.
Note: A review of the world’s literature reveals that David Abramson, MD, chief of Ophthalmic Oncology Service at Memorial Sloan Kettering Cancer Center, is perhaps the world’s most experienced specialist in treating retinoblastoma. He is credited with developing several procedures that have spared many infants from enucleation. More recently, this procedure has been modified to be used for bilateral retinoblastoma.
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Bass is a Distinguished Teaching Professor at the SUNY College of Optometry and is an attending in the Retina Clinic of the University Eye Center. She has served as an expert witness in a significant number of malpractice cases, the majority in support of the defendant. She serves as a consultant for ProQR Therapeutics.
1. Atkinson J, Anker S, Bobier W, et al. Normal emmetropization in infants with spectacle correction for hyperopia. Invest Ophthalmol Vis Sci. 2000;41(12):3726-31. 2. Kim HS, Yu DS, Cho HG, et al. Comparison of predicted and measured axial length for ophthalmic lens design. PLoS One. 2019;14(1):e0210387. 3. Semeraro F, Forbice E, Nascimbeni G, et al. Ocular refraction at birth and its development during the first year of life in a large cohort of babies in a single center in northern Italy. Front Pediatr. 2020;7:539. |

