 |
Although light flashes are a common symptom of vitreal-retinal traction, we must consider other etiologies such as prodrome to migraine as well. Persistent flashes in the absence of evidence of these two common causes should alert the clinician to search for other etiologies. Just as traction of the vitreous on the retina often produces light flashes, compression of any component of the visual pathway by a mass lesion can also result in light flashes. Reliance on confrontation visual fields to rule out visual pathway disorders may have a catastrophic outcome (such as discussed previously in our November 2023 column).
Case
A 15-year-old girl presented with a complaint of headaches and flashing lights. Best-corrected visual acuity (BCVA) was recorded as 20/20 OD and 20/20 OS. The external examination elements, including pupils, motility and confrontation visual fields (VFs), were recorded as normal, as was a dilated fundus exam (DFE). Because of the symptoms of headaches and flashing lights, a visual field screening was performed. The results were labeled as “marginal/questionable” (Figure 1). The eye clinician recommended a follow-up exam in one year.
 |
|
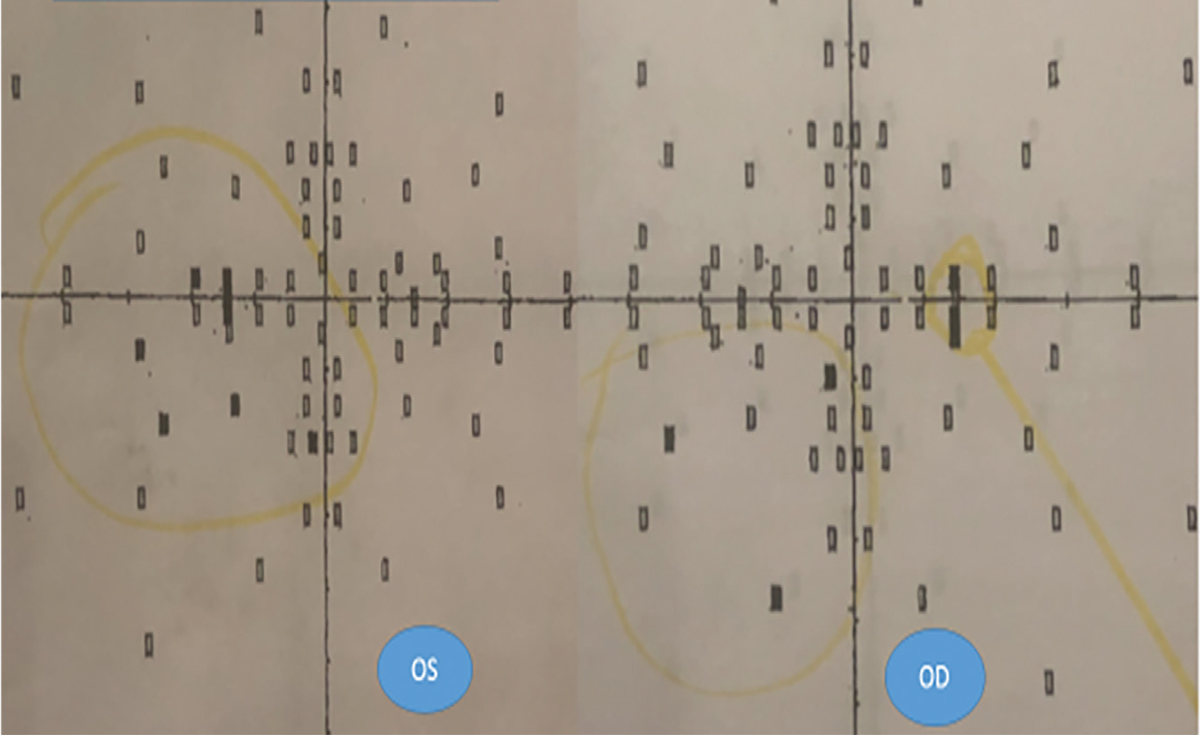
Fig. 1. VF screening on first visit. Yellow circles drawn years after exam. Click image to enlarge. |
The patient returned one year later, still complaining of headaches and flashing lights. She also complained of occasional problems focusing. VA was 20/20 OU with -0.25 sphere in each eye. The external exam, including motility, pupils and confrontation VFs, was recorded as normal. The diagnosis was myopia and paresis of accommodation. Again, a follow-up exam was recommended in one year. At age 17, the patient presented still complaining of headaches and flashing lights. BCVA was still 20/20 in each eye with -0.25 sphere in each eye. The DFE was recorded as normal, including disc margins and periphery. Her diagnosis remained unchanged, and the patient was told once again to return in one year.
One year later, headaches and flashing lights as the chief complaints were again recorded. VA was still correctable to 20/20 with a -0.25 sphere in each eye. Once again, the external exam, including pupils, motility and VFs, were recorded as normal. The fundus exam noted normal disc margins and periphery in each eye. It was recommended that the patient return again in one year.
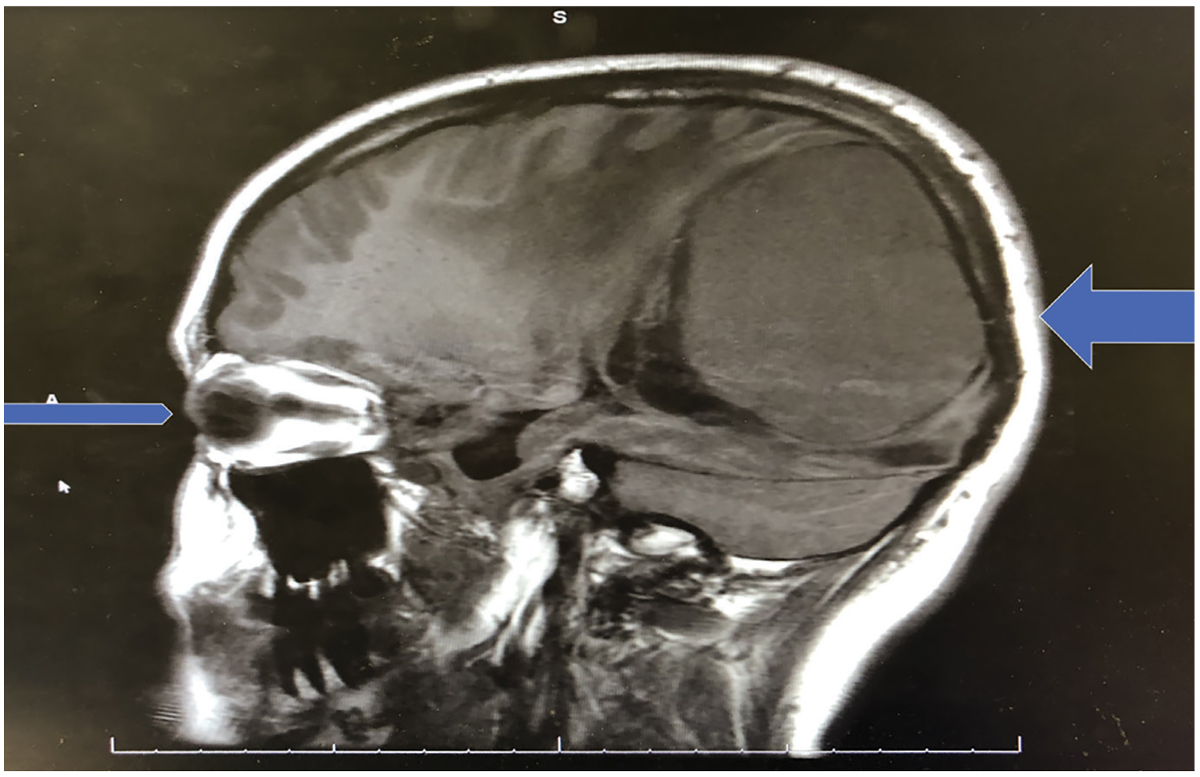
Nine months after the eye exam at age 18, the patient presented with family members to the emergency room (ER) of a major hospital. The initial diagnosis was “altered mental status, severe drowsiness and acute blindness.” An MRI that was ordered revealed a giant parietal-occipital meningioma 8x8x7cm, primarily on the right side of the midline (Figure 2). A craniotomy and resection in a nine-hour operation was performed the next day. This first procedure removed 95% of the mass, and a shunt and gamma knife radiation were performed later for the remaining 5%. There has been no regrowth of the meningioma to date.
After the multiple procedures to remove the giant meningioma, which expanded to occupy about a third of the cranium, the patient had some remaining central vision in the right eye and finger-counting VA in the left eye. The patient was now in her early 20s, and her fields were very constricted, with no hope of her vision ever recovering. An OCT revealed virtually no remaining retinal nerve fiber layer in either eye. The patient learned to use a cane and relies on a seeing eye dog.
The eye clinician who examined the patient for four consecutive years as a teenager, as well as her pediatrician and an ear, nose and throat (ENT) specialist, were all sued for failure to appropriately evaluate the patient. The pediatrician referred the patient once to ENT for a complaint of hearing difficulty in her right ear, but neither physician ordered a CT or MRI.
You Be the Judge
In light of the facts presented thus far, consider the following questions:
- On the field screening performed at the first visit, were there findings suggestive of a problem affecting the visual pathways?
- Should the field screening on the first visit that was labeled as “marginal/questionable” have been repeated on subsequent visits?
- Is an MRI considered the standard of care for a patient complaining of headaches and flashing lights?
- Are confrontation VFs, recorded as being performed and normal on each of the four yearly visits, the standard of care?
- Do you believe that confrontation VFs were performed and were normal nine months prior to the ER visit, which revealed a meningioma occupying about a third of the cranium?
- Is the eye clinician culpable of malpractice?
- Could artificial intelligence (AI) have prevented the disastrous outcome?
Diametrically Opposed Opinions
One of us (JS) was requested to review all the available records and opine whether the eye clinician met the existing standard of care on each of the four visits.
On the first visit, at age 15, the records noted that a VF screening was performed because of the chief complaints of headaches and flashing lights. Although the field screening was labeled as “marginal/questionable,” a careful review of the fields would reveal four missed points in the inferotemporal quadrant of the left eye and three missed points in the inferonasal quadrant of the right eye. This suggestive homonymous quadranopsia may be due to a post-chiasmal mass, affecting the superior optic radiations on the right side of the brain. The comment that the field results were “marginal/questionable” and not recognizing that the missed points were in corresponding quadrants is arguably not a violation of the standard of care. A like practitioner under like circumstances would, more likely than not, overlook this very subtle finding.
When the patient returned a year later still complaining of headaches and light flashes, the eye clinician relied on confrontation fields and did not repeat the automated visual field, even though on the first visit the doctor noted that the fields were performed because of the complaints of headaches and flashing lights. This is arguably a violation of the standard of care since automated VFs are non-invasive and can be obtained in several minutes. Similarly, when the patient returned at age 17 with the same complaints, the doctor again relied on confrontation VFs and did not perform automated perimetry.
The last exam performed by the eye clinician took place a year later, when the patient was 18, and the record revealed that the patient was still complaining of headaches and flashing lights. Details of the headaches and flashing lights were never recorded on any of the visits. For the fourth time, the retina was noted as normal, including evaluation of the optic nerve heads and the peripheral retina in both eyes. This was the third consecutive visit when automated VFs were not performed, even though automated VF screening was performed on the first visit because of the complaint of headaches and flashing lights.
 |
|
Fig. 2. This sagittal MRI images both the right eye and the parietal-occipital mass. Note the size of the mass relative to the size of the globe. Click image to enlarge. |
And then nine months later, the patient was rushed to the ER by family members and was diagnosed as having altered mental status, severe drowsiness and acute blindness. The MRI revealed a giant parietal-occipital meningioma. Bear in mind that meningiomas are nearly always slow-growing, strongly supporting the opinion that the tumor was present and slowly increasing in size over many years. Could confrontation fields have been normal nine months earlier? An underappreciated advantage of automated VFs is that it furnishes proof that fields were performed on a specific patient on a specific date.
There is no way to prove that confrontation VFs were performed and performed appropriately; most clinicians would conclude in such a case that either confrontation VFs were not performed or not performed appropriately. Unlike automated VFs, confrontation VFs can be influenced by human factors such as hunger, thirst, incoming text messages, number of patients in the waiting room, complaining about waiting time, etc.
The two experts who defended the eye clinician argued that many teenagers were incapable of performing automated VFs and that confrontation VFs are adequate to meet the standard of care and to detect large brain tumors. To quote these experts: “Automated visual fields in patients under the age of 18 are often notoriously unreliable.” In contrast, most eye clinicians will argue that teenagers, because of spending hundreds of hours playing video games, are far better than our typical, elderly glaucoma patients at performing meaningful VFs. One of these experts noted “confrontation visual fields when done appropriately with special techniques can be highly reliable.”
In this case, there is no evidence that any “special techniques” were ever incorporated in the confrontation visual fields. The two experts also opined that there was no substantial evidence on the four visits that neuroimaging was required since a mere complaint of headaches—a very common symptom—does not require a CT or MRI. This is arguable but a noninvasive, rapid and inexpensive and available procedure such as automated VFs clearly was indicated.
When a visual field device that incorporates AI reaches the market, consider it, since AI will easily recognize such a subtle homonymous quadranopsia and other retinal, optic nerve and visual pathway patterns.
The case was settled prior to a jury trial for several million dollars.
Takeaways
There were many lessons learned from this case, such as:
- When VFs are marginal or questionable, repeat them!
- Even in these uncertain VFs, there may be a pattern suggestive of a visual pathway abnormality: Look for it!
- “Normal” confrontation VFs give the patient and doctor a false sense of security.
- Don’t ignore symptoms and complaints that patients have repeated.
- When a patient consistently complains of headaches and flashing lights, think brain tumor!1
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Bass is a Distinguished Teaching Professor at the SUNY College of Optometry and is an attending in the Retina Clinic of the University Eye Center. She has served as an expert witness in a significant number of malpractice cases, the majority in support of the defendant. She serves as a consultant for ProQR Therapeutics.
1. Botterell EH. Early recognition of brain tumors. Postgrad Med. 1964. 36(4):297-300. |

