 |
A 45-year-old presented for new glasses because of reduced vision at distance and near in both eyes. He had no other symptoms or contributory history. Best-corrected visual acuity (BCVA) was 20/25- in each eye at distance and near with only a minimal change in prescription. The external exam including confrontation visual fields (VFs) was recorded as normal. Slit lamp revealed mild cataracts in each eye. IOPs were normal, as was the fundus exam in each eye.
The ophthalmic clinician advised the patient that all was well except for the mild cataracts and that cataract surgery may be indicated at a future date. As instructed, the patient returned in two years for a re-evaluation. The record indicated that the patient had the same symptom of reduced vision in both eyes as two years earlier. BCVA was again noted as 20/25- in each eye, and the external exam was unremarkable. Slit lamp exam revealed mild cataracts in both eyes as noted two years earlier.
Bear in mind that this patient, with obsessive compulsive disorder (OCD), kept a detailed health diary with notes about each visit with all health clinicians. He included his symptoms, tests performed, results of both the tests and the exam as explained by the doctor, differential diagnoses, medicine prescribed, possible side effects of the medicine and dates of future visits.
On his second visit with this eye clinician, the patient recorded and dated in his diary blurred vision, worse in the left eye than the right eye and worse in the left field. His chief complaint was far more detailed in his health diary than the chief complaint recorded by the examining doctor.
As recommended by this eye doctor, the patient presented another two years later. He complained that his vision was a bit worse than the previous visit but he denied any other symptoms. Best-corrected VA was 20/25- in each eye, and the external exam was again recorded as within normal limits. Slit lamp exam revealed mild cataracts once again in each eye but noted as slightly worse than before. IOPs were normal and unchanged, and the fundus exam noted the same 0.3 cup-to-disc ratio in both eyes as previously recorded. Refraction revealed a very mild change in the prescription, but the patient decided to get a new frame and lenses. He was reassured that there was no serious problem and again told that the cataracts will eventually need to be removed at some distant date.
As recommended, the fourth visit occurred two years later. The patient was previously seen in 2002, 2004, 2006 and now in 2008. He never missed an appointment!
 |
|
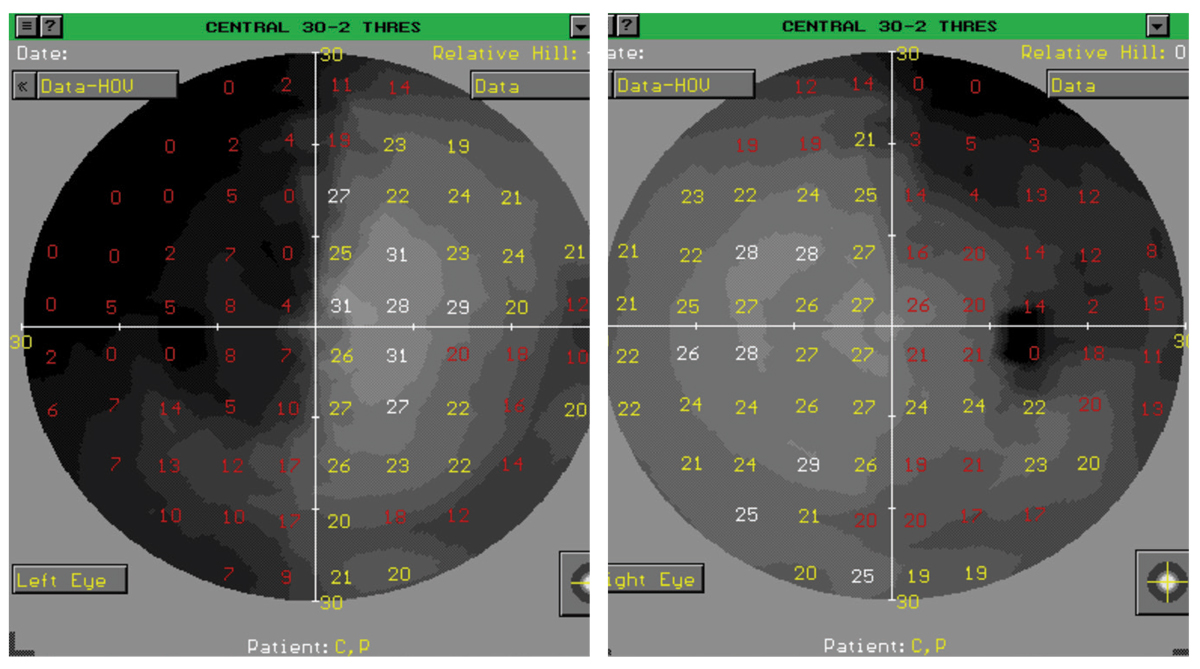
Fig. 1. Fields from a different patient than the case described who had vague complaints. Note the temporal loss in the left eye is worse than the temporal loss in the right eye. Click image to enlarge. |
Surgical Input
During the eighth year following his initial complaint, the patient felt his vision was worsening. He eventually decided to obtain a consultation from a highly respected cataract surgeon. Part of the initial consultation was a screening VF, which indicated a bi-supero-temporal field defect, somewhat worse in the left eye.
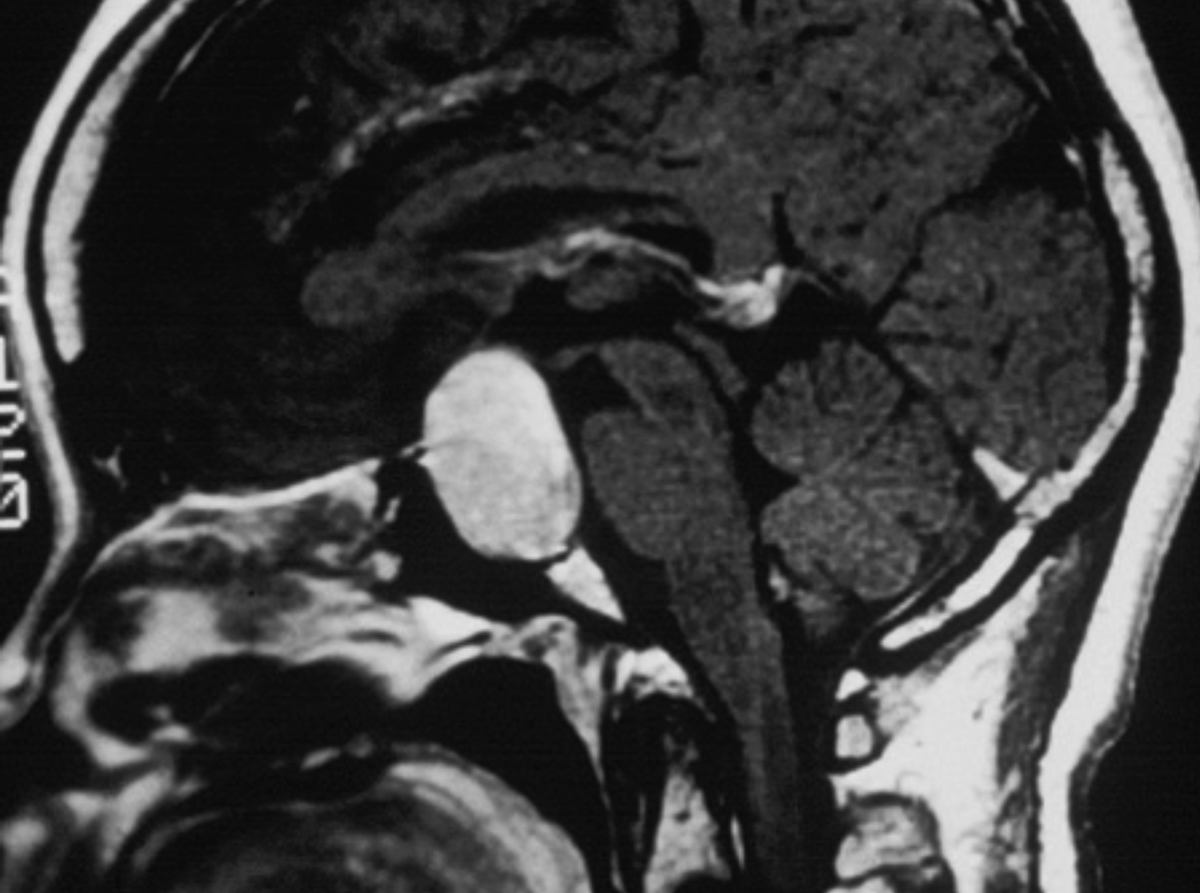
The cataract surgeon then performed a routine dilated exam and informed the patient that his cataracts were only mild and certainly did not require surgical removal. The surgeon then told the patient that the VF screening test strongly suggested a problem in the head. Threshold VFs were then performed and confirmed the screening field results, which were highly suggestive of a pituitary tumor and that an MRI should be obtained. Within several days, the MRI was obtained and the neuro-radiologist confirmed a large pituitary adenoma.
The patient was immediately referred to a prominent neurosurgeon at a major medical center. This specialist discussed two very different surgical approaches. The first was much less invasive, required an incision above the upper teeth or through the nose and then through the sphenoidal sinus and did not require major brain surgery. The second procedure, described to the patient as “cracking the skull” was more invasive, had a better chance of success but included greater risk.
The patient decided to have the transsphenoidal adenomectomy surgery. Scanning the patient a day after surgery revealed that much of the tumor remained. The patient obtained several neurosurgical consultations, and all agreed that the more invasive, and more dangerous, procedure was now indicated. One month after the “successful” removal of the remaining mass, the patient died in the hospital, never regaining consciousness after the second procedure. Cause of death: complications of the second surgery.
You Be the Judge
- Should the eye clinician have considered a diagnosis beyond mild cataracts?
- Should an automated VF screening be obtained on any of the four visits?
- Do confrontation VFs give the doctor and patient a false sense of security?
- Did the eye clinician take and record a detailed history of chief complaints?
- Is the eye clinician culpable of malpractice?
- Would you judge the doctor culpable of malpractice if the patient did not keep a detailed health diary?
Follow-up
Family members knew the patient had a health diary and reviewed it several weeks after the funeral. They then contacted a malpractice attorney who accepted the case. An optometrist (JS) was asked to review all the documents, the all-important diary and furnish an opinion.
The entry by the patient relating to the second visit stated, blurred vision, worse in the left eye than the right eye and worse in the left field, which appeared to have been totally disregarded by the eye clinician. Since the patient recorded this chief complaint in his health diary, we assume this was also reported to the doctor. Since the fundus exam was noted to be normal, blurred vision in the left eye worse in the left field strongly suggests a temporal field loss in the left eye. With a normal retinal exam, etiologies beyond the globe must be considered.
 |
|
Fig. 2. Mid-sagittal MRI from a different patient that demonstrates a pituitary adenoma. This current patient underwent successful surgery, and the fields returned to normal. Click image to enlarge. |
Our Opinion
Pituitary adenomas are common tumors, and if they grow large enough below the chiasm, the inferior nasal fibers at the optic chiasm will be impaired and typically result in a superior-temporal field loss, usually bilateral, but not always symmetric (Figures 1 and 2). Many patients with early to moderate bitemporal field loss are unaware of the VF defect, most likely due to the fact that the temporal field loss of the right eye is filled in by the normal nasal field of the left eye and the temporal field loss of the left eye is compensated by the normal nasal field of the right eye. With both eyes open, the field is essentially normal, and many patients do not cover one eye and then the other.
The records of far too many malpractice allegation cases of failure to detect brain lesions contain “confrontation VFs recorded as normal.” In several of these cases, it is unclear whether confrontation VFs, although recorded as normal, were ever performed. We believe that normal confrontation VFs can give the doctor and patient a false sense of security.
Many patients in their mid-forties have mild cataracts but most are asymptomatic. Persistent symptoms require a complete work-up, and this includes automated VFs. One could argue that this patient could still be alive if automated visual fields were performed and interpreted properly.
Without the health diary documenting the blurred vision, worse in the left eye than the right eye and worse in the left field, the malpractice allegation would be far more tenuous.
Prior to a jury trial, the case was settled for an undisclosed amount, but in the realm of a million dollars. A jury trial could have resulted in a much larger award.
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Bass is a Distinguished Teaching Professor at the SUNY College of Optometry and is an attending in the Retina Clinic of the University Eye Center. She has served as an expert witness in a significant number of malpractice cases, the majority in support of the defendant. She serves as a consultant for ProQR Therapeutics.

