 |
Plaquenil (hydroxychloroquine, Sanofi) is considered the drug of choice by rheumatologists for a host of autoimmune disorders. Although it has a relatively safe systemic profile overall and Plaquenil macular toxicity is not common, rheumatologists, internal medicine physicians and especially optometrists and ophthalmologists must remain cognizant of its potential for irreversible visual devastation.
As a general rule, each patient’s risk depends on daily dose and duration of treatment. The standard 400mg daily dosage taken continuously results in a calculated cumulative dose at seven years of slightly over 1,000g. Formulas for daily dosage based upon body weight exist but are rarely considered.
The American Academy of Ophthalmology (AAOph) guidelines recommend patients receive a baseline examination within the first year of Plaquenil use and an annual screening after five years of use when the cumulative dose begins to approach 1,000g.
Case
A tall, quite slender, 25-year-old white female fashion model presented for updating of her contact lenses. Her health history revealed treatment with Plaquenil 400mg/day for approximately 15 months, prescribed by her rheumatologist for both rheumatoid arthritis and Hashimoto’s thyroiditis. Her best-corrected visual acuity (VA) with -1.50 spheres in each eye was recorded as 20/20+. An external exam including Amsler grid in each eye was unremarkable. A dilated fundus exam revealed normal discs with 0.2 cup-to-disc ratios OU, a normal macula with a foveal reflex in each eye and normal peripheral retina in each eye. An SD-OCT of the disc and macula were obtained and was interpreted as normal.
 |
|
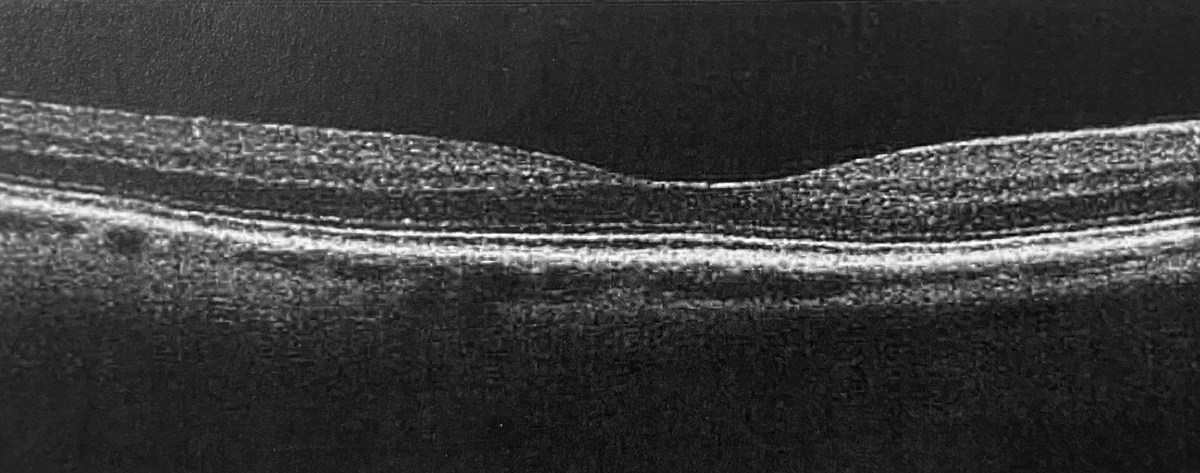
The first OCT was obtained by the first eye doctor. This horizontal scan of the posterior pole of the right eye was taken with Optovue. Click image to enlarge. |
New fashionable glasses were prescribed, as well as daily wear contact lenses. The eye clinician reviewed the possibility of irreversible retinal damage secondary to the drug Plaquenil. The doctor recorded that he discussed daily dosage and cumulative dosage and advised the patient to return yearly for retinal exams.
The patient returned a year later for a follow-up exam as recommended. Because she had since moved, this exam took place in a different office by a different doctor. She reported that she was still being treated for Hashimoto’s thyroiditis with Plaquenil 400mg/daily by the same rheumatologist for a total of about two and half years. Best-corrected VA was 20/20- OU, the external exam including confrontation visual fields was normal, Goldmann IOPs were 15mm Hg OU and a dilated fundus exam (DFE) was also normal OU. SD-OCT of the disc and macula was interpreted as normal in both eyes.
About four months later, the patient began having difficulty with her vision, worse in her right eye with both her glasses and contact lenses. As a fashion model, she was very attuned to color and also complained of slightly impaired color vision in both eyes. She returned to the first doctor, who gave her the detailed information about possible retinal problems with Plaquenil, and reported that she was still on Plaquenil 400mg/daily for a total of nearly three years.
Best-corrected VA was now 20/25 OD and 20/20 OS. Amsler grid revealed several small zones of missing lines around the central fixation point in the OD only but loss of contrast of the central lines in both eyes. A DFE revealed subtle pigmentary changes in both maculae, worse in the right eye.
The doctor immediately arrived at the diagnosis of Plaquenil macular toxicity and called the patient’s rheumatologist, who told the patient to stop the Plaquenil. An appointment with a highly respected retinologist was scheduled. One week later, the retina specialist fully evaluated the patient and agreed with the diagnosis of Plaquenil-induced macula toxicity and advised the patient never to consume Plaquenil again. The retinologist also informed the patient that there was no effective treatment at the present time to reverse the damage already done.
Shortly afterwards, the patient initiated malpractice litigation against the rheumatologist for prescribing too high a dosage of Plaquenil and both eye doctors for failing to perform comprehensive evaluations that could have detected the drug toxicity earlier.
You Be the Judge
- Was the patient—a successful fashion model who, at 5’ 10”, weighed only 99lbs—on too high a dosage of Plaquenil?
- Should the patient’s weight have been a red flag to the rheumatologist and to the two eyes doctors?
- Did the first eye doctor interpret the SD-OCT correctly?
- Did the second one interpret the SD-OCT correctly?
- Is bull’s eye maculopathy, diagnosed with ophthalmoscopy or fundus autofluorescence (FAF), an early sign of toxicity?
- When Plaquenil is discontinued, might the retinopathy still progress?
- If the patient were Asian and not Caucasian, would the recommended exam be modified?
Our Opinion
One of us (JS) was asked to review the case by the attorneys representing the first eye doctor.
After reviewing all the records and other available information, I opined that the first eye doctor met the existing standard of care. This doc corrected visual acuity to 20/20+ in each eye, performed an Amsler grid, which was normal in each eye, did not find any abnormalities with a dilated fundus exam, obtained an SD-OCT, which was interpreted correctly as normal, and counselled the patient about retinal risks of Plaquenil over time.
Could this doc have gone beyond the standard of care and performed baseline fundus photography, FAF, multifocal electroretinographs (mfERGs), comprehensive color vision and 10-2 visual fields?
It is unclear which test or tests are most sensitive to detect early Plaquenil toxicity, and hence it can be argued that it is in the patient’s interest to perform several of these tests. There exists literature that demonstrates that mfERGs are most sensitive for detecting early Plaquenil toxicity, but mfERGs are rarely available in ophthalmic practices.
Most surveys reveal that well more than half of ophthalmic clinicians have access to SD-OCT; hence, this easy-to-perform, objective test—which rarely requires dilation—is a component of the existing standard of care in managing patients on Plaquenil.1 However, the performance of a test alone does not meet the existing standard of care.
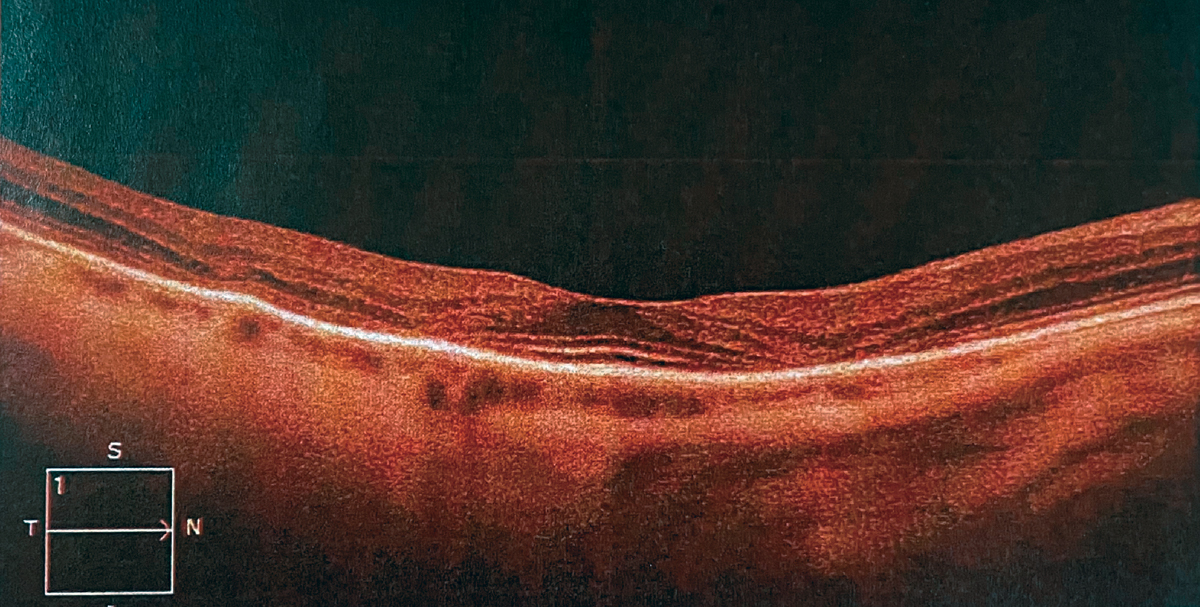 |
The second OCT was performed a year later by the second eye doctor. This horizontal scan of the posterior pole of the right eye was taken with a Zeiss. Click image to enlarge. |
In addition to OCT and mfERGs, fundus autofluorescence is the third objective test often recommended. The AAOph 2016 Revised Screening Guidelines for Plaquenil Toxicity states that one of these three objective tests should be performed. The same Guideline also lists VA, a DFE and a 10-2 SITA standard visual field with a white stimulus but a 24-2 SITA standard or a 30-2 with a white stimulus for Asian patients. It is generally agreed this population develops Plaquenil toxicity initially outside the macula.
Although I (JS) was not asked to render an expert opinion about the second eye doctor, who also performed an SD-OCT, it should be noted that the test was incorrectly interpreted as normal. The thin bright line above the retinal pigment, termed the photoreceptor integrity line (PIL), the ellipsoid zone or the IS/OS junction, should be continuous throughout the entire scan.
In this case, the PIL was present under the fovea but clearly missing to either side of the fovea. This is a finding highly suggestive of early Plaquenil toxicity and is most often encountered prior to bull’s eye maculopathy detection with ophthalmoscopy or fundus photography.
Additional Comments and Follow-up
Plaquenil-induced macular toxicity is a somewhat uncommon clinical encounter and is very rare in the first several years of treatment, such as in this case. Plaquenil should be discontinued immediately if maculopathy is detected. Note that the maculopathy sometimes continues to progress for several years even after the drug is discontinued due to the slow clearance of the drug from the retina and retinal pigment epithelium. It has even been reported to progress for up to two decades after discontinuation.2
We will never know with any certainty whether this patient’s low weight contributed to the early onset, but it is certainly plausible. The case against the rheumatologist was reportedly settled early on for an undisclosed amount. The case against the first eye doc was dropped, primarily because the OCT was performed and interpreted correctly. The case against the second eye doc went forward and was based upon his misinterpretation of the OCT.
One could argue that if he did not perform an OCT, the case against him would not have been pursued. The outcome is unknown at the present time.
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Diana Geraghty and Dr. Sherman are presently composing a manuscript to be submitted for publication tentatively entitled, “Imaging—Friend or Foe in Malpractice Allegations?”
Dr. Bass is a Distinguished Teaching Professor at the SUNY College of Optometry and is an attending in the Retina Clinic of the University Eye Center. She has served as an expert witness in a significant number of malpractice cases, the majority in support of the defendant. She serves as a consultant for ProQR Therapeutics.
1. Marmor MF, Kellner U, Lai TY, et al.; American Academy of Ophthalmology. Recommendations on screening for chloroquine and hydroxychloroquine retinopathy (2016 revision). Ophthalmology. 2016;123(6):1386-94. 2. Pham BH, Marmor MF. Sequential changes in hydroxychloroquine retinopathy up to 20 years after stopping the drug: implications for mild vs. severe toxicity. Retina. 2019;39(3):492-501. |

