 |
A 33-year-old in her 33rd week of pregnancy presented to the emergency department (ED) of a small rural hospital. Her chief complaint was severe headaches on her left side. She reported no history of trauma. Several ER doctors evaluated her and obtained a CT scan, which was read as normal. This small rural hospital did not have an MRI, and the nearest facility with one was about 25 miles away. No contusions on the face were noted.
The diagnosis that was then arrived upon was migraines, and she was treated with Imitrex (sumatriptan, GlaxoSmithKline) for the headaches and improved hydration. No neurologist was available in the ED at that time to evaluate the patient. Her OB-GYN was not contacted and the ED doctors did not attempt to obtain an OB-GYN consult at that time.
She was not hospitalized but was evaluated the next day by her ear, nose and throat doctor, who was affiliated with the small rural hospital and hence had access to the records from the ED. He reviewed the CT scan from a day earlier and diagnosed sinus involvement and treated her with oral antibiotics.
 |
|
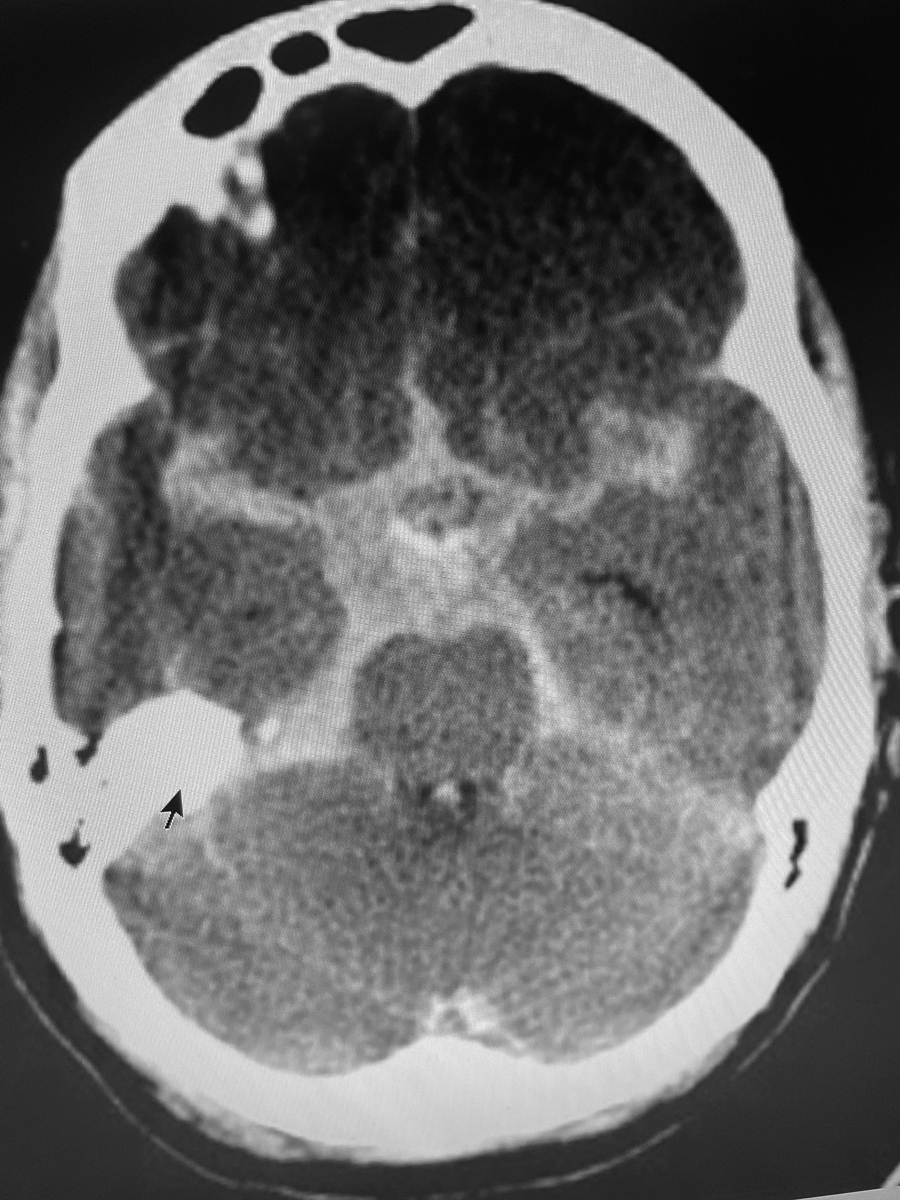
On CT scans, blood appears white. Depicted here is a subarachnoid hemorrhage (black arrow) on the right side of the brain from a different patient. There was no such obvious bleed in this tragic case. Click image to enlarge. |
Presentation
Three days later, she was examined by her optometrist, who obtained a history, then recorded normal VA in both eyes and a normal fundus evaluation. The OD noted that both pupils reacted to light. He observed anisocoria, and occasional diplopia in extreme positions of gaze was identified, which were not present on previous exams by the same optometrist. The patient reported to the OD the normal CT scan several days earlier, as well as the diagnoses of migraine headaches, dehydration and a sinus infection and the treatments prescribed. When asked, she stated that she was taking the meds as prescribed. The optometrist concluded that the very pregnant woman should have a neurological evaluation ASAP, but he could not obtain one directly because of the patient’s health insurance rules.
However, he was able to arrange for the patient to be seen by her primary care physician (PCP) early the next morning. He faxed over all his records and stressed in his note that he observed anisocoria for the first time and highly recommended a referral to neurology ASAP. The PCP evaluated the patient the next morning, was aware that the patient was referred by her optometrist based upon an exam the previous day, reviewed the history, performed an exam and arranged for the next available neuro consult several days later.
Tragically, the patient died two days before the scheduled appointment with the neurologist. The cause of death was determined to be a subarachnoid bleed. All attempts to save the near-term baby were unsuccessful. The woman and her unborn daughter were buried together.
Not surprisingly, everyone involved in the care of this patient in the last week of her life was sued for malpractice, including the hospital and the personnel in the ED and the radiologist, who concluded that the CT scan was within normal limits. As anticipated, the ENT MD, OD and patient’s PCP were all included in the lawsuit.
You Be the Judge
What caused the subarachnoid bleed? A pre-existing aneurysm that burst because of the physiological and/or psychological stress of pregnancy? Unreported head trauma secondary to spousal abuse? Is anisocoria nearly always caused by serious disorders in the brain?
Let’s blame the EMR? OK, but why? Is this a case of bad disease and not bad doctors?
If you were the OD, what would you have done?
Our Opinion
One of us (Dr. Sherman) reviewed all the available information and concluded that the optometrist met the existing standard of care. It is important to note that migraine headaches are considered one of the more common causes of anisocoria, but rare etiologies, such as subarachnoid hemorrhages, are occasionally encountered. In malpractice allegations, the legal system often considers what “a like practitioner would do under like circumstances.” In this case, a like practitioner would likely have done the same.
The OD was aware that the patient was dismissed by the MDs at the local hospital but still was quite concerned and reasoned that a neurologist may be able to determine the cause of the patient’s symptoms and clinical findings. If the patient’s health care plan would have allowed for a direct referral to a neurologist, at least one day would have been saved and it is possible that the tragic outcome would have been avoided.
Plaintiff’s experts for the surviving family members argued that a lumbar puncture should have been performed and may have been diagnostic of a bleed. The nearest MRI was 25 miles away at a larger hospital, but a lumbar puncture could have been performed in the ED during the same visit.
Generally Accepted Standard of Care for Emergency Room Physicians
|
Outcome
The case against all the defendants was settled prior to a jury trial. The insurance companies for all the defendants contributed to the final global award, which was under a million dollars. The insurance company for the OD contributed a very small fraction of this amount.
Comments
Hormonal changes and hemodynamic stress during pregnancy may cause an increase in the risk of aneurysm development and rupture (especially during the last trimester). The incidence of subarachnoid hemorrhage during pregnancy is one in every 10,000 patients, a rate five times higher than in nonpregnant woman.1
The emergency department MDs may or may not have been culpable in this case, but this can be best argued by dueling expert witnesses on both sides in the same specialty. Did the radiologist miss the bleed? Should the radiologist have recommended an MRI? Experts in neuroradiology for the plaintiff and for the defense can render their opinions after reviewing the CTs.
A female neurologist friend/colleague who learned about this case opined that OB-GYN should have been consulted in the ED before dismissing the patient. An MD/PhD neuroradiologist friend who frequently testifies in malpractice cases opined that “CT scans can be normal in some patients with subarachnoid hemorrhage, and especially if the headaches commenced greater than 48 hours prior to the scan.”
A review of the PCP’s deposition revealed several problems in the existing health system and in EMRs. The PCP testified that she could not order an MRI, but it could be ordered by the neurologist who never had the opportunity to examine the patient because of the death several days before the scheduled exam.
The PCP also testified that she never saw the faxed records from the optometrist but recognized that the patient was referred by her optometrist. She went on to explain in her deposition that the faxed records went into the “tank or holding tank” of their EMR system, and she was never educated about how to obtain the fax or how long the fax would remain in the holding tank before being transferred to the patient’s records. The technician who typically performed this task was not present for the 8am appointment.
During the deposition, the PCP was not asked the obvious question: If she had reviewed the referring optometrist’s records and report during her evaluation, would she have done anything differently such as immediately have the patient transferred to an ED of a major medical center? We will never know.
If this case went to trial, a sympathetic jury may have found some or even all of the defendants culpable of malpractice, and the jury award could have perhaps been in the many millions.
Although the OD met the standard of care, this case demonstrates in general that multiple MDs who examine a patient before you do may be wrong and you have the opportunity, if not the responsibility, to get it right. An immediate referral by the OD to the ED of a major hospital may just have altered the outcome in this tragic case.
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Bass also holds the position of Distinguished Teaching Professor at the SUNY State College of Optometry. She is a Diplomate of the American Board of Optometry. She is an attending in the Retina Clinic of the University Eye Center and currently serves as the residency supervisor for the Residency in Ocular Disease at SUNY. She has no financial disclosures.
1. Fox MW, Harms RW, Davis DH. Selected neurologic complications of pregnancy. Mayo Clin Proc. 1990;65(12):1595-618. |

