 |
Amblyopia is the most common reason for vision loss in kids and reported at 1% to 5% in various population studies.1,2 Most clinicians and experts consider amblyopia as monocular reduction of best-corrected visual acuity in the absence of any observable pathology. The two most common amblyogenic factors are constant unilateral strabismus and/or significant anisometropia. Without such an amblyogenic factor, the clinician must consider a series of less than obvious disorders such as subtle corneal involvement, a maculopathy not easily observable with ophthalmoscopy and, most problematic of all, an optic nerve or visual pathway disorder that could result in blindness or even death.
Case
A 13-year-old Caucasian girl presented with her mother for her first eye exam complaining of blurred vision in her right eye. Her ocular and general health history were unremarkable, and no family history of unusual visual problems were reported to the technician who obtained the history. Unaided visual acuity (VA) was 20/40 OD and 20/20 OS. The external exam performed by the optometrist—pupils, color vision, motility, cover test, confrontation visual fields—were recorded as normal. A refraction yielded no significant refractive error and pinhole did not improve the VA in the right eye. Goldmann IOPs were measured as normal, and a dilated fundus exam (DFE) was unremarkable. Routine fundus photos were taken of the posterior pole OU.
The doctor diagnosed amblyopia and suggested no intervention such as glasses, patching or eye exercises. According to the patient and her mother, the doctor told her she would likely “grow out of” the lazy-eye condition and recommended a follow-up in one year.
The teenager went on with her busy schedule—school, sports, friends and a boyfriend—without any noticeable change. She had an occasional headache, which was relieved by Tylenol (acetaminophen, Johnson & Johnson). However 50 weeks later, she experienced flashing lights in class in her right eye only, followed by a further loss of vision several minutes later. Panicked, her mom scheduled an emergency appointment with the same doctor the next morning. VA on this second visit was now 10/400 in the right eye but remained at 20/20 in the left. The external exam revealed an afferent pupillary defect OD compared with normal pupils on the first exam. The fundus exam on this occasion revealed a slightly pale disc in the right eye only.
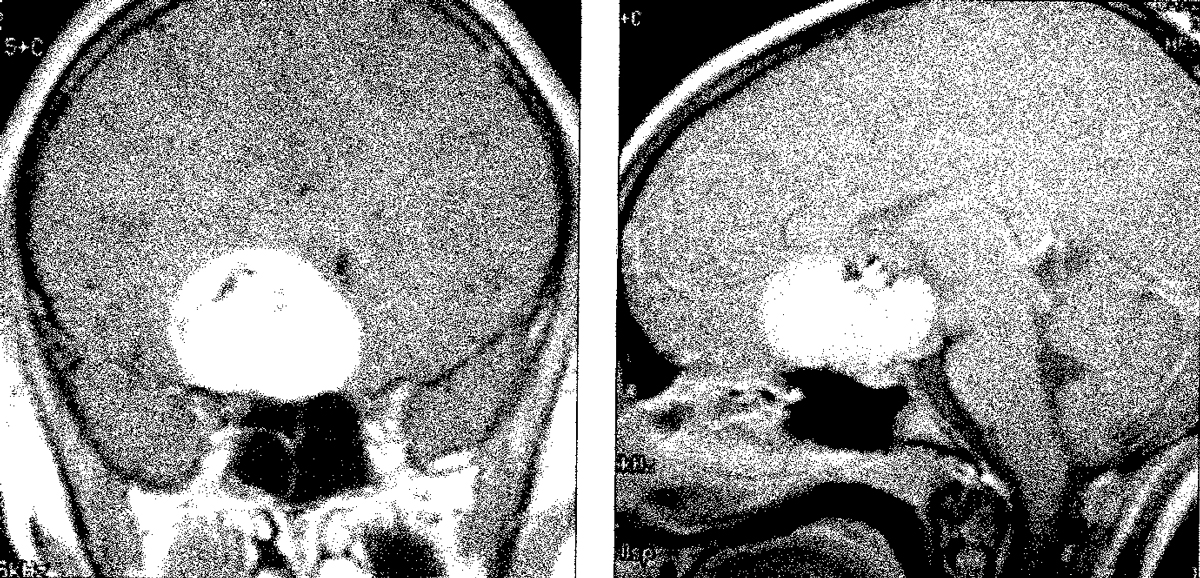
A series of referrals resulted in an MRI and arterial angiography later that same day. The imaging revealed a 3.5cm prechiasmal mass on the right side that compressed part of the chiasm. The patient was then referred to a highly rated pediatric neurosurgeon associated with a prestigious children’s hospital.
 |
|
A coronal (left) and mid-sagittal (right) MRI. Several experts testified that a year earlier, the tumor would have been far smaller and treatable with gamma knife radiation. Click image to enlarge. |
You Be the Judge
In light of the facts presented thus far, consider the following questions:
- Since confrontation visual fields and the DFE were both normal on the first visit, was the diagnosis of amblyopia justified?
- Since the doctor did not find a constant unilateral strabismus or significant anisometropia, should the doctor have considered other possible diagnoses?
- Was the doctor correct when he stated to the patient and the parent that she would likely “grow out of” the lazy-eye condition?
- Do normal confrontation visual fields give both the doctor and patient a false sense of security?
- Is the doctor not culpable of malpractice because both confrontation visual fields and a DFE were both normal?
Follow-Up
The patient and her parents listened carefully as a team of pediatric neurosurgeons discussed the risks and benefits of surgery to remove the brain tumor. No other options, such as gamma knife radiation, were recommended because the tumor was just too large to be treated successfully. The family was told that death, paralysis, loss of smell and blindness were possible as consequences of the major surgical procedure. But if all went well, the surgical intervention would perhaps result in normal VA and a near normal field in the left eye.
The parents consented and surgery was scheduled for the next morning. By all indications, the surgeon performed flawlessly. But two hours after surgery, marked complications arose, most notably elevated intracranial pressure. After noninvasive medical intervention failed, a shunt was inserted to relieve the pressure build-up but also failed. With informed consent from the parents, removal of part of the frontal lobe was performed and proved successful.
The patient woke up the next morning after two surgical procedures, both with general anesthesia, opened both eyes and saw nothing—not a thing again except for vague light perception. Her boyfriend visited her in the hospital, was told that his girlfriend will likely be blind forever and never returned. Her girlfriends did better and lasted about a month. The distraught parents were very supportive but realized everything had changed forever. They soon found a highly regarded law firm and began working with a young, sympathetic but aggressive attorney.
I (JS) was contacted because of previous publications about the diagnosis and misdiagnosis of amblyopia. I reviewed all the information available, including the depositions of the eye doctor and the technician who took the original history and from the mother and the patient. Of particular interest, the doctor testified that he did perform confrontation visual fields and both the patient and the mother supported this assertion. The doctor then testified that with normal confrontation visual fields, there was no reason to perform an automated visual field, a device he did have in his office. He also stated that he performed color vision testing, which was normal. However, under oath he was forced to admit that he performed the color vision test with both eyes open and hence did not compare the “affected” eye to the “normal” eye. Note that color vision loss does not occur in amblyopia and hence monocular color vision could be diagnostic.
The patient and mother testified that they told the technician that the vision loss in the right eye was rather recent— information that the technician did not note on the record. Also, the doctor never independently inquired about this critical point from the patient and mom during the exam. Recognize that doctors hold responsibility for their technicians and other office personnel via the legal doctrine of vicarious liability. Not surprisingly, a review of school records indicated that VA in the past was always normal.
The Outcome
Unlike most malpractice cases, this case did go to a jury trial, and the verdict of culpability was reached on a Friday afternoon. Several local newspapers published the story over the weekend and the name of the culpable doctor was revealed. The doctor had two kids in the same high school as the blind patient and within days everyone at school knew whose father was responsible for their blind classmate. The final verdict was $9.2 million, believed to be the largest ever against an optometrist.
Our Opinion
This landmark case occurred a quarter of a century ago. If modern day technology were used, many subtle abnormalities could have been detected. For example, OCT (not widely available at the time) can detect photoreceptor disorders invisible to ophthalmoscopy and, more importantly, a reduction in the retinal nerve fiber layer (RNFL) and ganglion cell complex that may be secondary to a brain tumor compressing the optic nerve. Reliance on confrontation visual fields has proven disastrous in a series of well-publicized malpractice cases. Automated visual fields, even a screening visual field, should be performed when there is no explanation for a patient’s symptoms or reduction in best-corrected VA, in all patients regardless of age. In the June 2023 installment of You Be the Judge, a pituitary adenoma in a middle-aged male was missed on four visits over eight years and resulted in death. The minor reduction in VA to 20/25 in each eye was attributed to mild cataracts but automated visual fields were never performed.
Silver Lining
This unfortunate case was widely distributed in the optometric press at the time and included the names of the optometrist and the expert witnesses. I (JS) had numerous lectures canceled, but far more importantly, a handful of clinicians in the years following contacted me and reported that knowledge of this case changed their professional behavior and some young “amblyopic” patients were demonstrated to have brain tumors.
Earlier diagnosis and appropriate treatment generally result in better outcomes. As a neurosurgeon once testified, “It is far easier to remove a grape from the brain than a grapefruit.” Learning from the mistakes of others can avoid such disasters.
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Bass is a Distinguished Teaching Professor at the SUNY College of Optometry and is an attending in the Retina Clinic of the University Eye Center. She has served as an expert witness in a significant number of malpractice cases, the majority in support of the defendant. She serves as a consultant for ProQR Therapeutics.
1. Meng Z, Fu J, Chen W, et al. Prevalence of Amblyopia and associated risk factors in Tibetan grade one children. Ophthalmic Res. 2021;64(2):280-9. 2. Kuwera E. Lazy eye (amplyopia). Johns Hopkins Medicine. www.hopkinsmedicine.org/health/conditions-and-diseases/lazy-eye-amblyopia. Accessed September 29, 2023. |

