 |
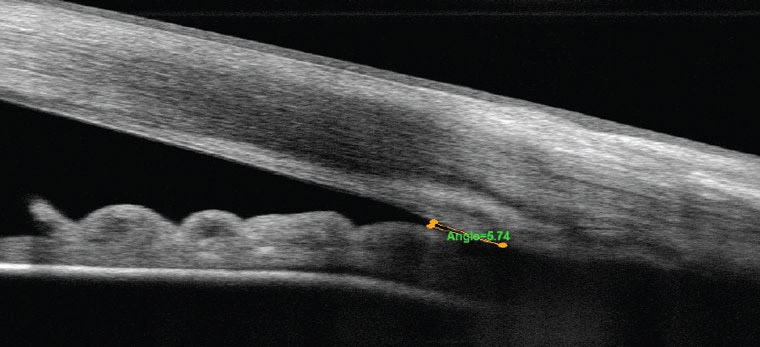
| This meta-analysis identified 10 primary angle-closure risk factors, including cataract, body weight, retinal nerve fiber layer thickness, hyperlipidemia, cholesterol, triglyceride, malondialdehyde and short-term antidepressant exposure.Photo: Michael Cymbor, OD. Click image to enlarge. |
Previous studies have confirmed the major risk factors associated with primary angle-closure glaucoma (PACG), including intraocular pressure (IOP), anterior chamber depth and axial length, but the social factors and serological indicators remain unclear. In a new study, researchers summarized primary angle-closure glaucoma (PACG)-related factors across different dimensions and found 10 additional factors, including cataract, short-term antidepressant exposure and increased levels of hyperlipidemia and triglyceride.
Through a review of 45 studies, 30 factors were included in the meta-analysis. PACG was found to be significantly associated with body weight, retinal nerve fiber layer thickness, cataract, hyperlipidemia, total cholesterol, triglyceride, malondialdehyde and short-term antidepressant exposure, which may help in understanding the causes of primary angle-closure glaucoma, the authors noted.
The authors hypothesized that cataract might be involved in the pathogenesis of PACG by affecting lens thickness. “With the progression of cataract, the lens tends to thicken bi-directionally. During the development of PACG, an increase in lens thickness or a more anterior position of the lens could result in angle crowding and a greater predisposition to pupillary block,” the authors explained in their article for Optometry & Vision Science. “Furthermore, as lens thickness increases with age, the anterior chamber angle becomes shallower, pupil block may be more likely leading to an increased incidence of PACG. In addition, reduction of IOP has been observed in patients with the angle-closure disease after cataract surgeries, suggesting that the treatment of cataract is of clinical significance for primary angle-closure glaucoma management.”
Regarding short-term antidepressant exposure, “most antidepressants relax the sphincter muscle of the pupil secondary to the anticholinergic properties, resulting in pupil dilation, cycloplegia, blockage of aqueous outflow and increasing of IOP,” the authors explained. “Mydriasis and cycloplegia could exacerbate the closure of iridocorneal angle in patients with shallow anterior chambers and narrow chamber angles, which then increases the risk of primary angle-closure glaucoma.”
Changes in retinal nerve fiber layer have been shown to be a major feature of the early stages of PACG, consistent with it being a sign for this disease, the authors noted.
Lastly, an association between hyperlipidemia and increased levels of triglyceride was found, suggesting that lipid metabolism disorders might influence primary angle-closure glaucoma. “A recent meta-analysis has also suggested that hyperlipidemia and increased blood lipid levels may be associated with increased risk of glaucoma and increased intraocular pressure,” the authors noted.
“Screening for relevant factors can help identify high-risk populations of PACG; however, identifying causal evidence between these factors and PACG and applying these potential factors to clinical diagnosis and treatment remain a great challenge for us,” the authors concluded. “More studies with larger numbers of cases and of high quality are warranted to validate the causal relationships between these factors and PACG.”
Wang Y, Dong X-X, Hou X-W, Pan C-W. Risk factors for primary angle-closure glaucoma: a systemic review and meta-analysis of 45 studies. Optom Vis Sci. September 26, 2023. [Epub ahead of print.] |

