 |
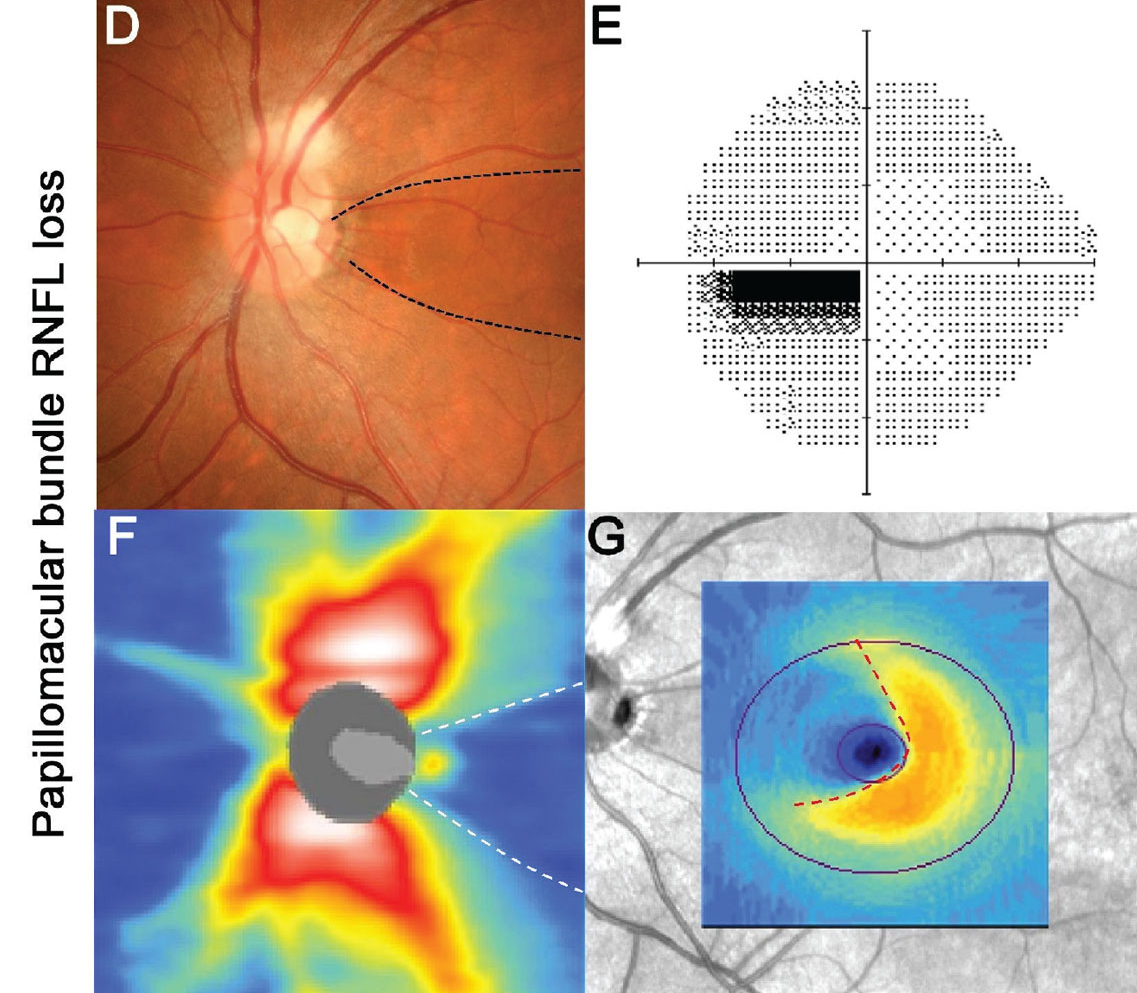
PPA-to-disc-area ratio (odds ratio; OR: 3.83), lamina cribrosa defect (OR 2.92) and central visual field defect (OR 3.56) were significantly associated with the papillomacular bundle defect. Photo: Henrietta Wang, BOptom. Click image to enlarge. |
The papillomacular bundle is a structure that plays an important role in central vision, and as such, it is expected that a defect there can affect the quality of life of patients quite significantly. Little is known about these defects in glaucoma. Researchers in South Korea investigated the frequency of papillomacular bundle defects in glaucoma patients with high myopia and its risk factors. They observed a defect in 59.8% of patients, which was significantly correlated with a larger parapapillary atrophy (PPA)-to-disc-area ratio, lamina cribrosa defect and central visual field defect.
The retrospective, cross-sectional study analyzed RNFL defect in 92 glaucomatous eyes with high myopia (axial length of 26.0mm or more or an average spherical value of −6D or less). After dividing the cohort into two groups with and without papillomacular bundle defect, the clinical characteristics of the groups were compared and analyzed. The mean age of the patients was 52.1 years, and there were 53 males and 39 females.
There was no significant intergroup difference in baseline or follow-up intraocular pressure. In this specific patient group, significant differences in PPA-to-disc-area ratio were found when dividing the population based on the presence or absence of a bundle defect.
“As larger PPA-to-disc-area ratio signals greater myopic deformation of the optic disc and peripapillary tissue, there must have been greater mechanical stress in the region of deformation,” the researchers wrote in their paper. “Therefore, the higher the myopia, the larger the PPA area that will be found; and notably too, the results of this study suggest that larger PPA area may be related to risk of RNFL thinning in the papillomacular bundle area.”
The study noted that swept-source OCT, which was used to image the lamina cribrosa, allows for deeper penetration of light for better delineation of more posterior structures of the optic nerve head and ocular wall, its penetration depth remains a limitation.
“Although we identified disc hemorrhage during follow-up, it is possible that instances that had occurred before follow-up or between follow-up intervals were missed,” the authors wrote. “Therefore, it is possible that the number of disc hemorrhages in the total patient group was low; thus, additional research based on a longer follow-up and a larger number of disc photo scans is necessary in order to more fully investigate the relationship between papillomacular defects and disc hemorrhages.”
The study concluded that “for highly myopic glaucoma patients, the presence of papillomacular bundle defect and/or lamina cribrosa defect possibly affecting the central visual field should be carefully evaluated.”
Huh MG, Shin YI, Jeong Y, et al. Papillomacular bundle defect (PMBD) in glaucoma patients with high myopia: frequency and risk factors. Sci Rep. 2023;13(1):21958. |

