Several macular and vitreomacular complications can present in patients with high myopia, two of the most common being neovascularization and atrophy. A recent study found that through choroidal quantitative assessment, three subgroups of high myopia can be characterized, which may help clinicians calculate a patient’s risk of developing MNV or atrophy.
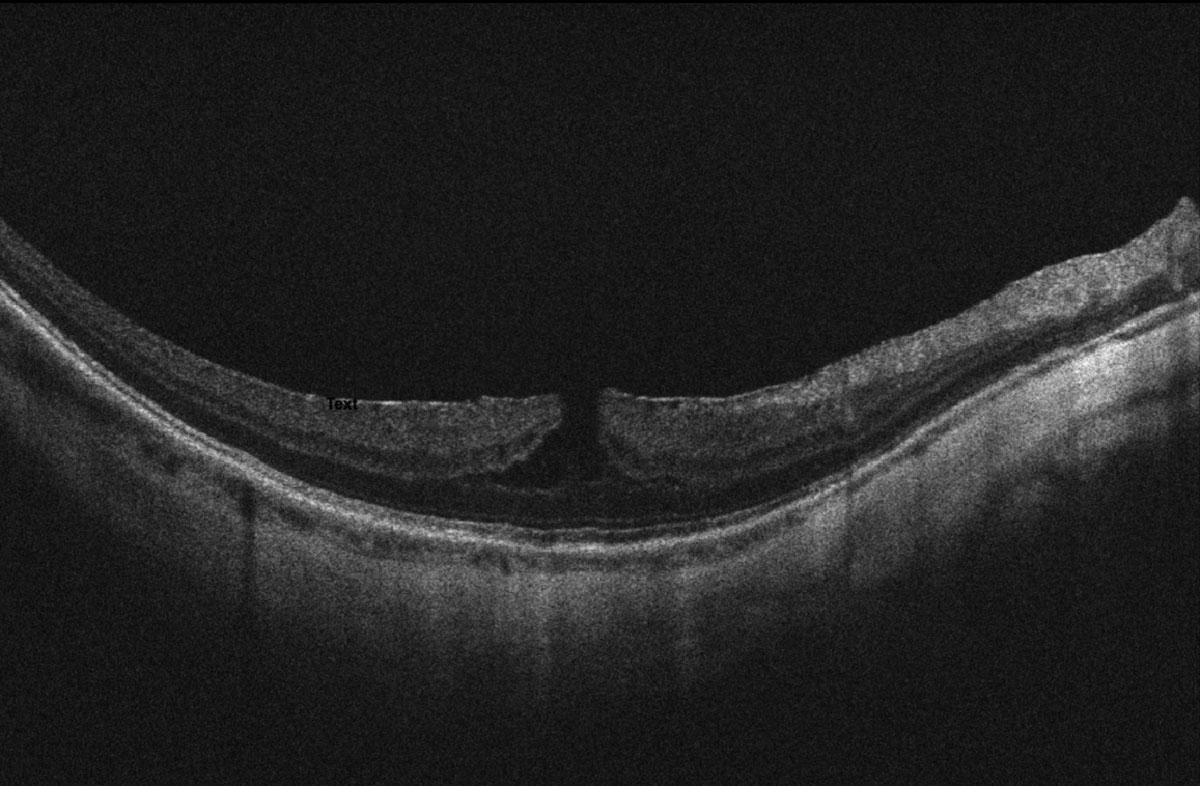 |
| Quantitative choroidal assessment can be used to categorize high myopes into three subgroups: high myopia without complications, with MNV or with macular or posterior pole atrophy. The MNV subgroup is characterized by intermediate choroidal thinning and a higher prevalence of round dome-shaped macula with sub-dome choroidal deepening. Photo: Alia Cappellani, OD. Click image to enlarge. |
A total of 190 eyes of 190 patients who met the inclusion criteria participated in the two-year retrospective case series. The investigators measured choroidal thickness (CT), the presence and subtype of dome-shaped macula and the presence and type of choroidal deepening in those with dome-shaped macula. Based on the data, they divided the cohort into three subgroups:
- Subgroup 1 (66 eyes): high myopia without complications
- Subgroup 2 (72 eyes): high myopia complicated by MNV
- Subgroup 3 (52 eyes): high myopia complicated by macular or posterior pole atrophy
All subgroups had similar age, gender and axial length distributions, the former two factors showing no significant effects on any performed measures. The most interesting finding, the researchers pointed out in their paper for Investigative Ophthalmology Vision & Science, was “the progressive reduction of CT values in all the subgroups from baseline to two-year follow-up.” They concluded that baseline CT could accurately distinguish between subgroups with and without myopic complications. More specifically, the authors explained that “a baseline CT cutoff of 40μm was significantly associated with the presence of myopic maculopathies, either considering MNV or non-neovascular maculopathy (sensitivity 0.83; specificity 0.74). Furthermore, a baseline CT cutoff of 30μm proved useful to segregate eyes complicated by MNV from eyes showing atrophy alone.”
This finding, the researchers add, agrees with prior reports suggesting that a thin choroid is a risk factor for MNV in highly myopic eyes.
Another factor evaluated in this study that varied significantly between subgroups was subtype of dome-shaped macula, a finding that presents in 9.3% to 20.1% of highly myopic eyes. This presented in 39% of cases in subgroup 1, 54% of which were represented by vertical dome-shaped macula and 48% which showed no choroidal deepening. In MNV eyes (subgroup 2), the prevalence of dome-shaped macula was similar, except 49% of these cases were characterized by round dome-shaped macula, and 55% showed sub-dome choroidal deepening. An equal number of eyes in subgroup 3 showed horizontal or vertical dome-shaped macula (53% and 47%, respectively), with 80% showing peri-dome choroidal deepening.
The researchers summarized the findings in their paper: “When dome-shaped macula is present, vertical subtype with sub-dome choroidal deepening is the most common combination in myopic MNV subtype, whereas non-neovascular pathologic myopia is mainly characterized by peri-dome choroidal deepening.”
They concluded that assessing choroidal measurements—specifically the extent and rate of CT and presence and subtype of dome-shaped macula—proved useful in this study for stratifying the risk of onset of myopic complications in high myopes. These metrics may play a role in improving diagnostic workup and treatment strategies, the researchers suggested.
Arrigo A, Aragona E, Bianco L, et al. The clinical role of the choroidal assessment in high myopia: characteristics and association with neovascular and atrophic complications. Invest Ophthalmol Vis Sci. 2023;64(12):16. |

