 |
|
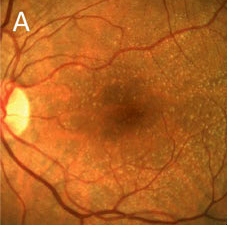
When detecting drusen smaller than 125µm, color fundus photography seems to allow for clearer visualization than OCT, researchers suggest. Click image to enlarge. |
As new technology reveals additional risk factors and clinical biomarkers for age-related macular degeneration (AMD), there is an urgent need to update severity classification systems, researchers of a recent study argue. Using retinal imaging, they determined that the genetic risk score of more than 3,000 adults was significantly associated with drusen and complete outer retinal pigment epithelium and outer retinal atrophy (cRORA). However, subretinal drusenoid deposits, hyperpigmentation and vitelliform lesions alone had no association with genetic risk score.
The researchers identified 3,368 adults between the ages of 36 and 99 (mean age: 63.4). The cohort underwent color fundus photography, spectral-domain OCT and a genetic risk score assessment using medical history and demographic data. The overall presence of AMD, based on color grading, in participants older than 55 was as follows:
no drusen: 0.4%
drusen <63μm: 15.9%
drusen 63µm to 125µm: 13.7%
drusen >125µm or pigmentary changes: 8.3%
late AMD: 1.6%
Furthermore, the presence of AMD features identified in those over 55 years was as follows:
OCT drusen: 27.5%
cRORA on OCT: 4.3%
reticular drusen: 3.2%
subretinal drusenoid deposits: 25.7%
The researchers noted, in accordance with prior studies, that the prevalence of drusen increased steadily with patient age. In the youngest age group (≥55 years), the prevalence of drusen was 1.3%, and in the oldest (≥85 years), it reached 9.6%, doubling with every 10-year age category.
“We showed clear and steady almost monotonic age-related rises in the prevalence of Beckman stages two and three representing early and intermediate AMD, respectively,” the researchers wrote in their paper for the British Journal of Ophthalmology. They also pointed out that color fundus photography seemed superior to OCT in identifying differences by age group in the frequencies of drusen.
“Notably, on color, the prevalence of drusen (any size) was higher than that seen on OCT in the younger age groups, and although it rose with age, the increase was shallow,” the researchers wrote. “On OCT, the prevalence of any drusen, which was around 16% in the youngest age band, rose steadily to 54% in the oldest age band. These color vs. OCT discrepancies mainly occurred in the detection of drusen <63µm.” For detection of drusen >125µm, color fundus and OCT performed comparably well.
One finding unique to this study was that subretinal drusenoid deposits or hyperpigmentation in the absence of classical drusen had no significant association with genetic risk score, but classical drusen alone showed a strong association. “This is not surprising since focal hyperpigmentation on its own can represent pathology such as past inflammation,” the researchers explained.
To sum up their findings, the study authors concluded, “Multimodal imaging-based classification has provided evidence of some divergence of genetic risk associations between classical drusen and subretinal drusenoid deposits. Our findings support an urgent review of current AMD severity classification systems.”
Hogg RE, Wright DM, Quinn NB, et al. Prevalence and risk factors for age-related macular degeneration in a population-based cohort study of older adults in Northern Ireland using multimodal imaging: NICOLA Study. Br J Ophthalmol. October 10, 2022. [Epub ahead of print]. |

