 |
A 48-year-old Hispanic male was referred to our ophthalmic emergency department from an outside trauma center with notable pain, tearing and bleeding due to a cut on his left lower eyelid. The night prior, he was involved in a motor vehicle injury, during which he recalled hitting the front windshield upon impact.
Case
The outside trauma center performed a CT scan, which was remarkable for mild left periorbital soft tissue swelling. There was a suspected associated nondisplaced fracture of the left lamina papyracea without any intracranial or retrobulbar hematomas. CT angiography of the neck was unrevealing. He had an ocular history of keratoconus and contact lens use. His surgical history included a cholecystectomy.
His visual acuity with pinhole on presentation was 20/50 OD and 20/30 OS. The pupils were equally round and reactive in both eyes with no relative afferent pupillary defect. Extraocular motilities had full range of motion OU without evidence of proptosis or enophthalmos. Intraocular pressures measured 17mm Hg OD and 15mm Hg OS.
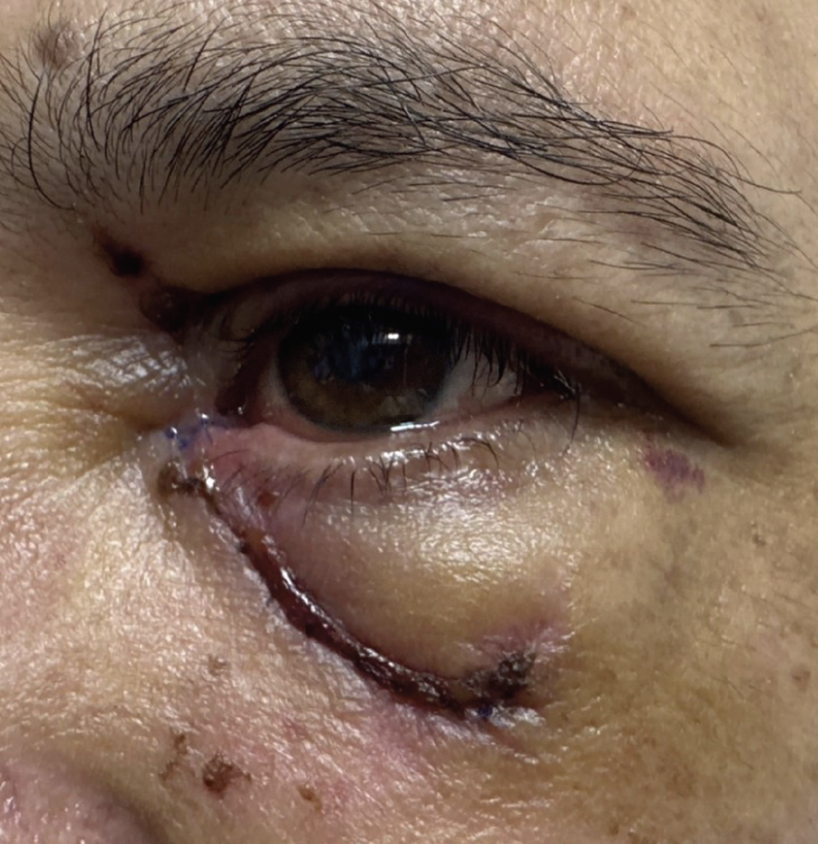
The external and anterior segment exam OD was unremarkable. On the left side, there was significant ecchymosis and erythema periorbitally with an inferior periorbital laceration. Upon closer observation, the left lower eyelid had a full-thickness tear medially to the puncta which involved the inferior canaliculus. The puncta was temporally displaced. A subconjunctival hemorrhage was present without conjunctival or corneal laceration. The dilated fundus exam was unremarkable.
The patient was diagnosed with a canaliculus-involving marginal laceration of the left lower lid. He was treated that day in the minor operating room for emergent repair.
 |
External photo on initial presentation to our ophthalmic emergency room. Click image to enlarge. |
Discussion
Partial- or full-thickness lid lacerations are precipitated by various causes of facial trauma and often concomitant with corneal or conjunctival lacerations, intraocular or intraorbital foreign bodies, open-globe injuries, orbital fractures, canthal tendon avulsion or disruption to the lacrimal system. The highest incidence of eyelid lacerations is found within the pediatric population and is frequently due to insults from bike handlebars, collisions with sharp objects, dog bites and falls.1 The most common insults in the adult population include trauma from physical altercations, motor vehicle accidents and sports balls.1
A methodical approach must be followed in evaluating an eyelid laceration. First, it is paramount to obtain a full detailed history, analyzing for the involvement of any bug or dog bites and organic or metallic material. A CT scan in 1mm or 2mm cuts, or an MRI if a non-metallic injury took place, may be an imperative ancillary test for an open globe injury, retained foreign material, fracture or intracranial injury. In these instances, prompt attention to and treatment of these findings is necessary before any external repair, such as that for an eyelid laceration. Further, a tetanus booster shot or systemic antimicrobial coverage may be of urgent need.
The next step is to perform wound irrigation with copious amounts of sterile saline. This may be followed by the removal of foreign particles and fibrin clots at the wound edges, reducing risk of infection or inflammation and promoting healing. Then, it is necessary to explore the wound’s depth and width of penetration to classify the cut. Gloves and a sterile cotton tip applicator can be used to analyze and explore the eyelid involvement. Topical anesthetics can aid in desensitizing the area.
 |
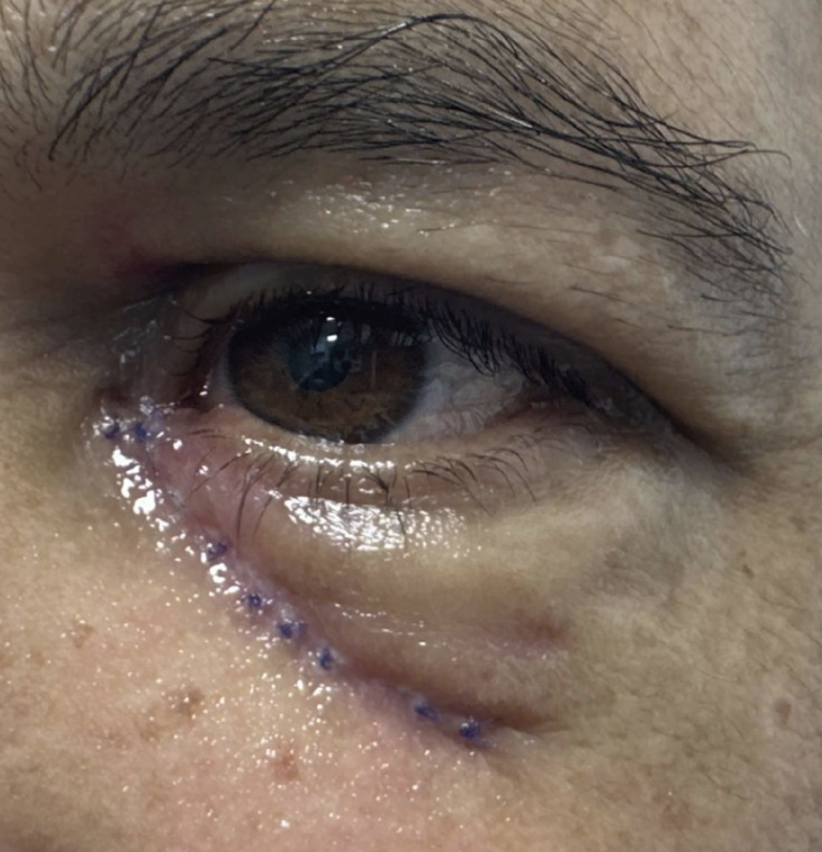
Five-day follow-up visit to evaluate the canalicular shunt sutures. Click image to enlarge. |
Eyelid lacerations can be classified into three groups: lacerations without eyelid margin involvement, with eyelid margin involvement or with nasolacrimal system involvement.1,2 Any lid margin involvement, visible orbital fat or damage to the lacrimal system, as confirmed by dilation and irrigation or probing, should raise immediate concern for an oculoplastic referral. Sudden-onset ectropion or ptosis, tissue disruption, orbital paresthesia or eyelid notching are all possible signs of eyelid margin involvement. Laxity, displacement, rounding or pouting of the medial canthus or puncta can signify lacrimal system involvement.
Surgical repair includes direct laceration closure via sutures, canthal release, a transitional flap, grafts and a variety of lacrimal stents to repair canalicular lacerations and avulsions.1-4 A referral within 24 hours is recommended to return drainage physiology to normal, reduce the risk of chronic epiphora and obtain good eyelid positioning postoperatively. However, one retrospective study of 334 patients divided into repair before and after 48 hours found no statistical difference in the treatment of canalicular lesions and suggested that surgery can be performed within six days of injury for confined cases.3
For patients with an eyelid laceration without margin involvement or visualization of orbital fat, understanding the eyelid anatomy and physiology is important for proper care. The eyelid skin is very thin and lacks subcutaneous fat, easily allowing for pockets of subepithelial edema.
The orbicularis oculi plays a key role in involuntary lid closure and may result in lagophthalmos with damage. This muscle is anterior to the orbital septum and orbital fat, which serve as important landmarks for the posteriorly placed levator aponeurosis. Therefore, as the injury deepens, orbital fat prolapse, septal perforation and ptosis may occur, all respective to their anatomical landmark.2 Structural damage to the eyelid may result in eyelid notching, irregular contour, shortening of the fornixes or entropion. Sequelae of anatomical changes include damage to the meibomian glands, exposure keratopathy or trichiasis. Further complications of eyelid lacerations include missed injury and infection.
Superficial lacerations involving less than 25% of the lid may be managed by tissue adhesives, antibiotics and monitoring alone.4 Broad-spectrum oral antibiotics can be prescribed, and topical antibiotics should be applied to the wound. A rabies prophylaxis shot may be used for patients who present with an animal bite. During follow-up, monitor for worsening edema or erythema, either of which would signify a possible infection.
 |
| Eighteen days after the insult following removal of the sutures. Click image to enlarge. |
Outcome
Our patient underwent same-day surgical repair and received a Mini-Monoka (FCI Ophthalmics) stent to aid in the repair of the left lower monocanalicular laceration. The distal edge of the stent was approximated near the lacrimal sac. Buried and superficial sutures were placed throughout the inferior periorbital dermal layers to approximate the epidermis and to appose the lid to the globe.
The patient was placed on amoxicillin-clavulanate 875mg-125mg by mouth twice daily for 10 days and bacitracin zinc/polymyxin B ointment twice daily.
At the patient’s five-day follow-up visit, the eyelid and stent appeared properly positioned. However, copious swelling and a high tear lake did not allow for clear distinction of a patent puncta at that time. He was instructed that the oral antibiotics were to be continued for five more days.
Eighteen days after initial insult, with decreased edema and improved ecchymosis, a clear indication of a patent puncta and a well-approximated lid allowed for the removal of sutures. The bacitracin zinc/polymyxin B regimen was continued for five more days following sutural removal.
The lacrimal system and periorbital skin continue to be monitored for drainage, epiphora and hyperpigmented scarring.
Dr. Bozung currently practices at Bascom Palmer where she primarily sees patients in the hospital's 24/7 ophthalmic emergency department. She also serves as the optometry residency program coordinator. Dr. Bozung is a fellow of the American Academy of Optometry and a member of the Florida and American Optometric Associations. She is a founding board member of Young OD Connect and serves on the editorial board for Review of Optometry. She has no financial interests to disclose.
Dr. Meyer is an ocular disease resident at Bascom Palmer Eye Institute in Miami. She graduated from the University of Houston College of Optometry in 2022.
|
1. Cade KL, Taneja K, Jensen A, Rajaii F. Incidence, characteristics, and cost of eyelid lacerations in the United States from 2006 to 2014. Ophthalmol Ther. 2022;12(1):263-79. 2. Cochran ML, Czyz CN. Eyelid laceration. StatPearls. Published November 27, 2022. www.ncbi.nlm.nih.gov/books/NBK470367/. Accessed May 10, 2023. 3. Chu YC, Wu SY, Tsai YJ, et al. Early versus late canalicular laceration repair outcomes. Am J Ophthalmol. 2017;182:155-9. 4. Chandler DB, Gausas RE. Lower eyelid reconstruction. Otolaryngol Clin North Am. 2005;38(5):1033-42. |

