 |
|
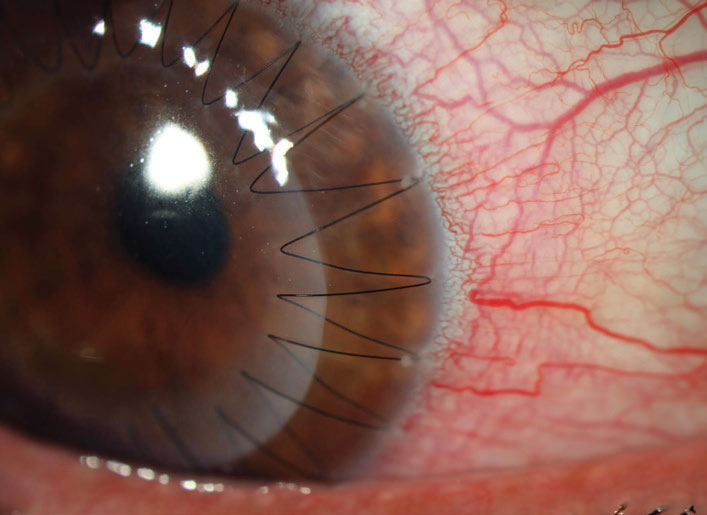
This study found several advantages of treating keratoconus patients with PK over DALK. Photo: Aaron Bronner, OD. Click image to enlarge. |
Lamellar surgeries have dramatically lowered the risk profile of corneal transplantation, but penetrating keratoplasty, if successful, can still be the preferred option in some cases. A new study sought to compare the two in their postoperative results. Including both PK and deep anterior lamellar keratoplasty (DALK), researchers sought to compare how both fare in terms of postoperative visual acuity, refraction, complications and further potential surgical interventions.
The retrospective, interventional study included 411 consecutive keratoconus eyes with a preoperative mean keratometry of greeter than 60D. Of those, 218 received PK and 193 received DALK.
After surgery, researchers found that visual acuity and refraction improved significantly for both groups when compared to baseline values. As well, keratometric astigmatism was comparable between the groups.
Regarding complications, suture-related ones were seen in 48.6% of PK eyes and 72% of DALK eyes. With graft rejection, incidence was 33.5% after PK and 19.7% after DALK. At final visit, 98.2% of PK grafts and 94.8% of DALK grafts remained clear.
Overall, PK resulted in better visual acuity and refraction when compared to DALK along with exhibiting fewer suture-related complications. The biggest downside of PK was a higher graft rejection rate when compared to DALK. Despite these differences, the two were comparable in graft survival rate.
The researchers provide some thoughts as for why DALK came up short in many aspects compared to PK. The lower postoperative visual acuity, they explain, could have due to light scatter caused by surgical interface.
They also found, in general, steeper corneal graft after DALK compared to PK, despite controlling for using similar trephination size and suture tension. With PK, intraoperative anterior chamber collapse and scarring instead results in a flatter graft.
DALK’s shortcomings can also be attributed to a high rate of suture loosening. This underscores the primary problem of the recipient cornea’s weak Bowman layer and thin stroma, resulting in an inability to resist suture tension. For the higher rate of observed loose sutures in DALK eyes, the researchers suspect it could be caused by surgeons’ preference to superficially place the sutures in hope to avoid perforation of thinner recipient corneas during the surgery.
While DALK displays its disadvantages, one major advantage of this procedure over PK is preservation of recipient endothelial cells. This results in no risk for endothelial graft rejection and a much lesser risk of graft failure from nonimmunologic endothelial decompensation. Researchers point out that they saw more incidents of graft rejection in PK than DALK, and this was because of endothelial graft rejections.
As a succinct way to distinguish the two procedures, the authors aptly note that “our results showed that visual and refractive outcomes as well as the rate of suture-related complications were significantly better after PK than DALK; however, the safety profile including risk of graft rejection and globe integrity after trauma favored the DALK procedure.”
Both options are safe, but since they do display unique differences in outcomes, the authors also advise that “patients undergoing corneal transplantation for advanced keratoconus should be counseled regarding these differences between the two techniques of keratoplasty preoperatively.”
Feizi S, Javadi MA, Karimian F, et al. Penetrating keratoplasty versus deep anterior lamellar keratoplasty for advanced stage of keratoconus. Am J Ophthalmol. 2022. [Epub ahead of print]. |

