 |
Q:
A 39-year-old male presented with uveitis and rather “sudden” loss of vision but no obvious fundus findings. Where should I begin?
The first question I often ask patients is, “When was the last time you had a complete physical with bloodwork?” says Cynthia Noorani, OD, of the Roswell Eye Clinic in Atlanta. This patient in particular reported he hadn’t been to any doctor since he was a child. Best-corrected vision was 20/50 OD and 20/100 OS, which had deteriorated over the previous week. Confrontation fields and pupils were normal. His color vision was abnormal in both eyes.
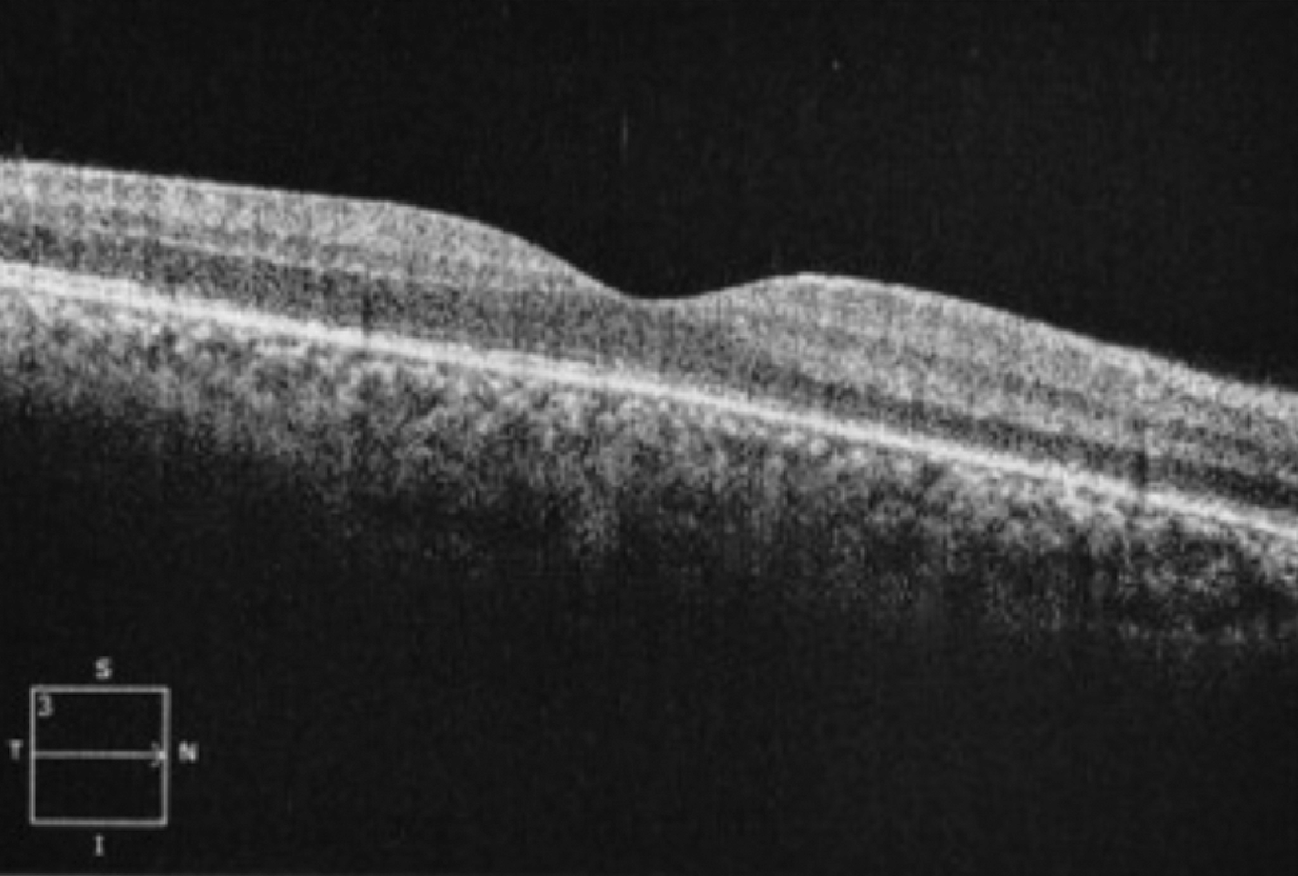
Slit lamp examination revealed an anterior and posterior uveitis, with no symptoms of light sensitivity. The retina was grossly normal, as were the optic nerves. The macular OCT showed very subtle retinal pigmented epithelium (RPE) thickening (Figure 1). His visual field showed bilateral central scotomas, confirming some variant of optic neuropathy.
 |
|
Fig. 1. OCT imaging with subtle areas of RPE thickening, or placoid chorioretinitis. Click image to enlarge. |
During the initial exam, the patient became emotional and asked if his general health could affect his eyes. “It was at this point that I had to ask some blunt questions related to sexual activity and any presenting signs, such as pain on urination or rashes,” says Dr. Noorani. He remained awkwardly silent during this line of questioning. A blood panel was ordered including testing for sexually transmitted infections, specifically an rapid plasma reagin (RPR), fluorescent treponemal antibody absorption (FTA-ABS) and venereal disease research lab (VDRL) for syphilis, NAT for HIV and IgM and IgG for herpes simplex. The patient agreed to the tests and started using a topical steroid drop for the uveitis.
A few days later, Dr. Noorani received a phone call from an infectious disease physician from the department of health. The patient tested positive for not only an active case of syphilis but also HIV with a CD4 count of 284—very close to reaching AIDS. He was started on intramuscular penicillin, and the infectious disease physician monitored him to see if his reaction to intramuscular would be enough before starting intravenous and HIV treatment. A retina specialist was consulted and confirmed that the findings on his OCT correlated with his syphilis diagnosis, known as placoid chorioretinitis.
Counting on Blood Count
Syphilis cases have been steadily rising in the United States, with an average of 12 million new cases per year in developing countries.1 The infectious disease is primarily caused by Treponema pallidum and is generally transmitted during sexual contact or congenitally in utero.1,2 Consider serological testing including RPR, VDRL and FTA-ABS in cases of vision loss and subtle neuro-ophthalmic findings as in this case.1,3
Syphilis is the third leading cause of an active interstitial keratitis, with herpes being the first.1 The most common ophthalmic finding—and maybe the only systemic sign—in syphilis is uveitis, which typically occurs six weeks after the primary infection.1 Another possible finding is Argyll Robertson pupils, which typically occurs late in the disease and may explain our patient’s small, sluggish pupils at his exam. The optic disc may be swollen either unilaterally or bilaterally and can be subdivided anteriorly or retrobulbar.1 Our patient had a subtle retrobulbar neuritis which explained his vision loss and abnormal color vision.
Syphilis is a very challenging clinical diagnosis because its presentation overlaps with many other etiologies. Dr. Noorani says she urges doctors to have a deeper conversation with patients in order to arrive at the correct diagnosis. Discussing the importance of getting updated blood work as part of a complete physical exam is something all practitioners should encourage.
“This patient had no idea he was also HIV-positive with a risky CD4 count that may have progressed to AIDS if he waited longer to be seen or get tested,” she notes. The patient returned about a month later with a best-corrected visual acuity of 20/20 OU and expressed immense gratitude for the care he received.
Dr. Ajamian is board certified by the American Board of Optometry and serves as Center Director of Omni Eye Services of Atlanta. He is vice president of the Georgia State Board of Optometry and general CE chairman of SECO International. He has no financial interests to disclose.
1. Lee AG, Bindiganavile SH, Wiley Z, Al-Zubidi N, Bhat N, Belushi FA. Ophthalmologic manifestations of syphilis. EyeWiki. eyewiki.aao.org/ophthalmologic_manifestations_of_syphilis. Published July 29, 2022. Accessed December 27, 2022. 2. Singh AE, Romanowski B. Syphilis: Review with emphasis on clinical, epidemiologic and some biologic features. Clin Microbiol Rev. 1999;12(2):187-209. 3. MedLine Plus. Syphilis tests. MedlinePlus. medlineplus.gov/lab-tests/syphilis-tests/. Accessed December 27, 2022. |

