 |
Q:
A patient reported left-sided head trauma and headaches after a recent motor vehicle accident. The referring provider indicated there was an inferior altitudinal defect in the left eye. The patient is under the care of a neurologist. What are the next steps?
Visual field defects are present in about 38% of patients with traumatic brain injuries (TBI), based upon a retrospective study.1 A recent meta-analysis stated that the prevalence was 6.6% in mild TBI cases and 39.8% in moderate to severe cases for visual fields of post-chiasmal origin.2 The severity of a TBI is defined using the following characteristics (Table 1).3
“Important case history elements to ask before evaluating functional vision symptoms include the onset of the injury, location of the injury and neurological status,” says Esther Han, OD, associate clinical professor and residency program supervisor of the vision rehabilitation residency with an emphasis on brain injuries at SUNY. If the accident was recent, either imaging or monitoring of any headache symptoms over a 24-to-72-hour period should be done to rule out a slow bleeding intracranial hemorrhage.3,4
 |
|
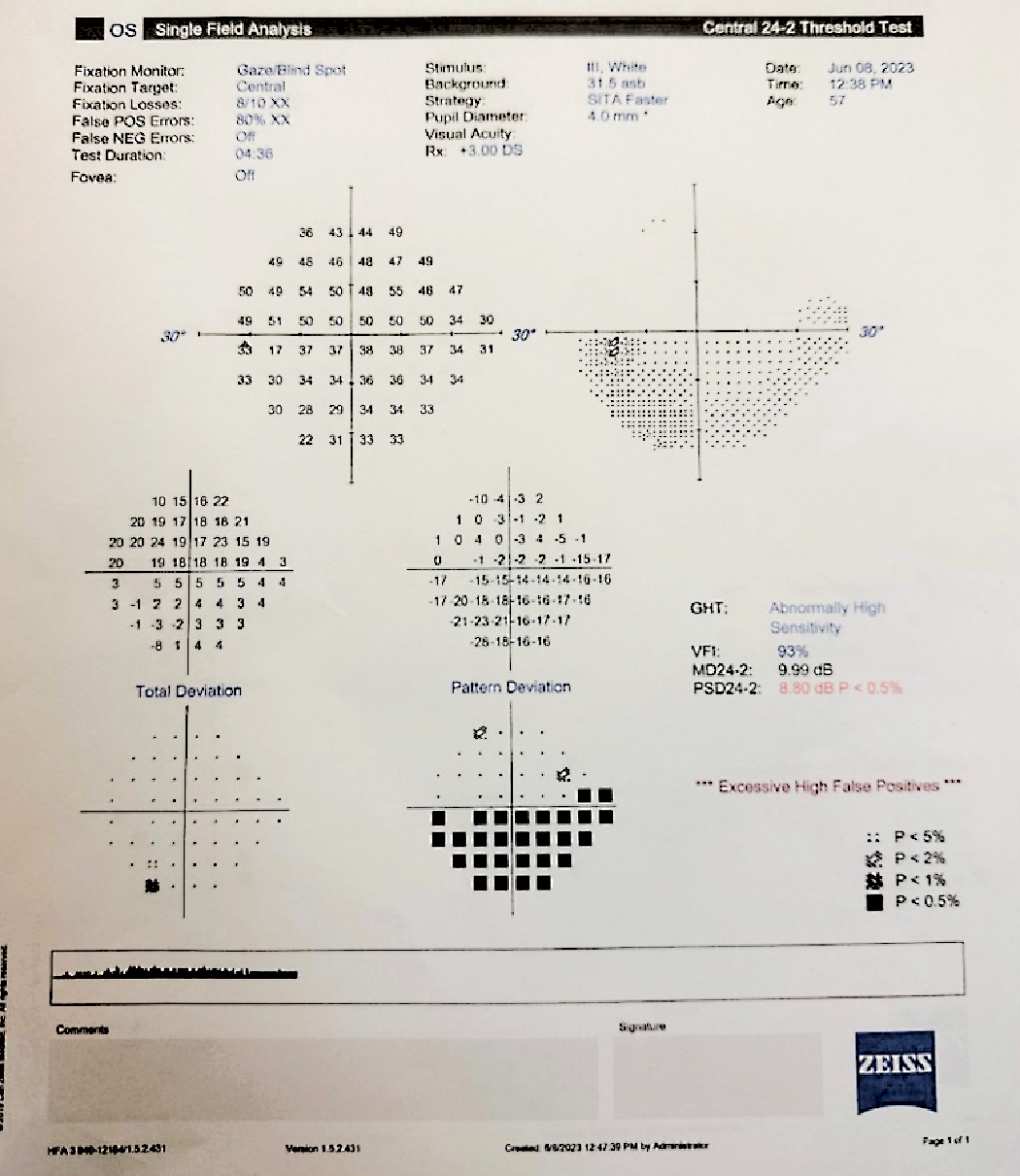
The left eye visual field of the patient with a left-sided head trauma secondary to a motor vehicle accident. Click image to enlarge. |
This patient may appear clumsier than before and/or may bump into or trip over things on the left side. Some additional visual field–related symptoms include experiencing restriction in their peripheral vision, loss of balance, dizziness, not feeling grounded and veering off to one side when walking.
Given the coup-contrecoup nature of the motor vehicle accident, where the patient’s brain jostles back and forth in the skull due to the force of the accident, the patient may additionally experience vision symptoms related to deficits in vergence, oculomotor and/or accommodative function, according to Dr. Han. She recommends performing the Convergence Insufficiency Symptom Survey (CISS), such as the one in the American Optometric Association’s Clinical Practical Guidelines, as a quick way to monitor symptoms. A score of greater than 21 for adults indicates the patient should be referred to a neuro-optometric rehabilitation/optometric vision therapy provider.
Neuro Evaluation
Typically, visual acuities will not be reduced, but there may be fluctuations in acuity and single letter acuities may need to be measured. Given that the patient in this case was hit on the left side of their head, Dr. Han notes that speech may be slower and less coherent during the recovery stage. “Perform a comprehensive ocular health assessment, including careful pupillary testing, motility, confrontation fields and a dilated exam, to determine the presence of any retinal, optic nerve or visual pathway abnormalities that require immediate referral and management,” she adds. “Since only one eye depicted visual field abnormalities, monocular color vision should also be performed as a baseline to monitor optic nerve function.”
In acute cases, light sensitivity will be a major symptom. Wearing a hat, visor or even sunglasses can help decrease this. During the examination, turning off the fluorescent lighting will significantly increase patient comfort.
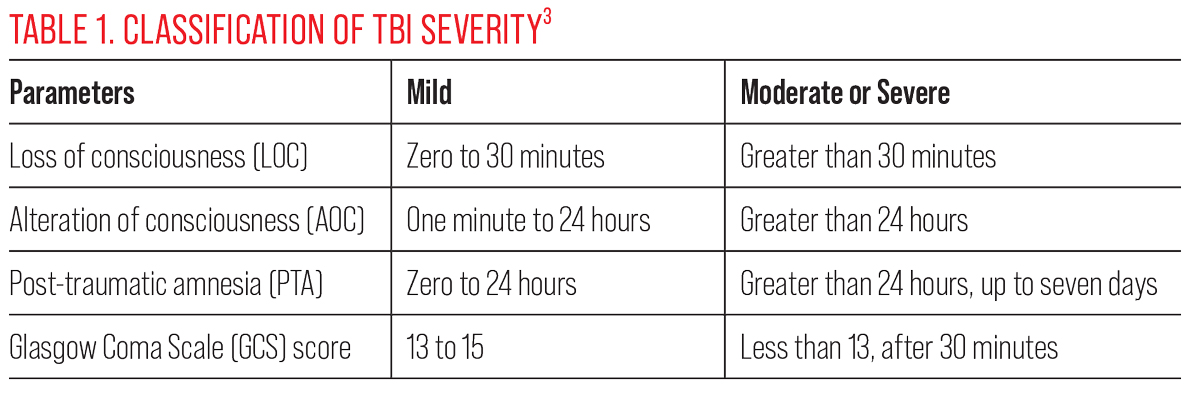 |
| Click table to enlarge. |
Management
In acute cases, the patient should be re-assessed in one to two weeks depending on the severity of symptoms. Repeat visual fields and other indicated baseline tests to monitor for change.
Because this patient experienced a mild TBI after the accident, the recovery period should be about two to four weeks. Should the patient report persistent symptoms, Dr. Han suggests that a referral to a physiatrist or rehabilitative medicine provider specializing in concussions would be indicated to manage any post-concussive syndrome-related issues. This provider will team with neuropsychology/cognitive therapy, physical/vestibular therapy, speech therapy and neurology to address persistent symptoms.
Ongoing visual symptoms such as light sensitivity or a CISS score that remains above 21 are indications that further treatment is required.
“Ophthalmic tints should be trialed should the patient report persistent indoor light sensitivity,” she notes. “Typically, 10% to 25% (absorption) blue, gray, brown tints are well-tolerated for indoor use.” Post-injury patients also report greater comfort with polarized lens sunglasses.
A referral for optometric vision therapy is indicated if the patient’s symptoms are interfering with their activities of daily living. “Should the visual field defects remain in the left eye, about 2PD to 5PD base-down yoked prism should be trialed for near work or as reading glasses to move images into the intact visual field,” Dr. Han says. “This will decrease the patient’s awareness of the relative field defect.”
Accurate charting is very important in motor vehicle accident cases with symptomatic patients, as records will be requested by various agencies such as no-fault insurance, short-term disability and attorneys.
Dr. Ajamian is board certified by the American Board of Optometry and serves as Center Director of Omni Eye Services of Atlanta. He is vice president of the Georgia State Board of Optometry and general CE chairman of SECO International. He has no financial interests to disclose.
1. Merezhinskaya, N, Mallia RK, Park D, et al. Visual deficits and dysfunctions associated with traumatic brain injury: a systematic review and meta-analysis. Optom Vis Sci. 2019;96(8):542-55. 2. Suchoff IB, Kapoor N, Ciuffreda KJ, et al. The frequency of occurrence, types and characteristics of visual field defects in acquired brain injury: a retrospective analysis. Optometry. 2008;79(5):59-65. 3. Silverberg ND, Iverson GL, Cogan A, et al. The American Congress of Rehabilitation medicine diagnostic criteria for mild traumatic brain injury. Arch Phys Med Rehabil. May 19, 2023. [Epub ahead of print]. 4. Homnick A, Sifri Z, Yonclas P, et al. The temporal course of intracranial hemorrhage progression: how long is observation necessary? Injury. 2012;4(12)3:2122-5. |

