The discussion of multifocal contact lenses usually results in the rendering of a blank stare from my students. They understand the concepts of multifocals, but are often indecisive in selecting lens designs for patients. They are also motionless when I discuss lens parameter changes to resolve patient’s visual complaints. To prescribe for success, the practitioner must understand a few fundamental concepts of multifocals.
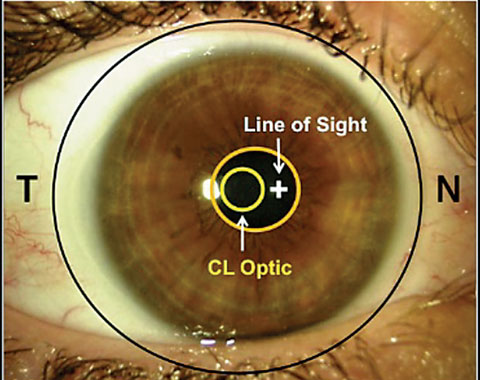 |
| Fig. 1. Line of sight offset (lens is pushed off temporally from scleral asymmetry). Photo: Matthew Lampa, OD. |
Distance and Near
First and foremost, unlike in multifocal spectacles, the distance and near powers of many multifocal contact lenses are organized in an annular center-and-surround configuration; thus, successful fitting of these lenses requires proper centration and careful monitoring of the patient’s pupil size. In the case of spectacles, however, when the patient views at distance, the only prescription the patient is viewing through is distance. The advantage of having a stabilizing nosepiece on spectacles is that the frame can be modified so that the multifocal can be positioned with the line of sight at the exact location that the patient’s eye would transcend down through to reach the lens’s near power area. In the case of multifocal contact lenses, the distance and near prescription areas reside within the pupil’s range so that both prescriptions can be viewed simultaneously. The only exception is alternating vision lens designs.
Commonly, the line-of-sight aligns the viewing target with the fovea through the nodal point, which must be taken in consideration when developing a multifocal lens design. Angle λ, which can be used to represent the difference between the visual axis and the pupillary axis, for the most part does not play a significant role in the success of single vision lenses because of their consistent power profile across the optical zone of the lens surface (Figure 2). This is true in the case of multifocal spectacles, but not so in multifocal contact lenses.
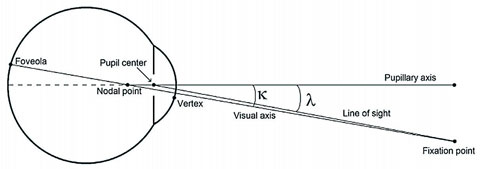 |
| Fig. 2. Difference between angle kappa and angle lambda. |
These specialty lenses rely much more on centration over the patient’s visual axis to achieve optimum multifocal optics in line with the patient’s line of sight; as such, without a stabilizing force to balance out the weight of the multifocal lens, successful centering of the optics in front of the pupil for the rays of light to accurately focus onto the retina may be difficult. Typically, line of sight is off-center by about 9 to 11 degrees, and can degrade vision due to the onset of coma and astigmatism. Furthermore, if the line of sight or lens centration is several millimeters off from the center of the pupil, full exposure to the multifocal optics portion of the lens will not be possible and can result in optical aberrations.
The lens design of a multifocal may also have a bearing on the fitting parameters: a center-near lens design will typically have a steeper profile in the center of the lenses surrounded by a flatter zone, while a center-distance lens design most likely exhibits a flatter profile centrally that is surrounded by a steeper profile. Using a topographer to measure the difference between the center of the pupil and the central ring of the videokeratoscopic image as it is centered over the patient’s line of sight can become increasingly important as the add prescription is increased.
Practitioners often experience difficulty aligning the line of sight because the multifocal soft lens is usually positioned temporally due to scleral asymmetry, while the line of sight is nasal to the geometric center of the eye (Figure 1). The nasal sclera is more elevated than the temporal scleral; as such, when a contact lens is placed upon the eye, the lens is pushed temporally. The optics of the contact lens can be displaced opposite to the amount of temporal decentration. This depends on the decentered optics, which is itself caused by the lack of centration. At times, the zone size can also be modified to improve the resultant visual acuity as long as there is a consistent power profile.
Fitting the Patient
Each multifocal lens available on the market today has a unique distance and near zone configuration, which can impact the wearer’s vision in distinctly different ways.
Practitioners should also keep in mind that the average pupil size varies from patient to patient, and also changes when exposed to both dark and light environments—facts that may further affect the selection of a lens design. Overall, multifocal lens design choice is controlled by pupil size: if the patient’s pupil is smaller than the zone configuration, vision will be impossible to view through the peripheral zone. Additionally, the older the patient is, the smaller their pupil area likely will be, due to senile miosis. As such, spreading the lens power across the distance and near zones is how most multifocal designs are created. This is typically done by measuring the patient’s pupil size under both scotopic and photopic scenarios during the initial fitting examination.
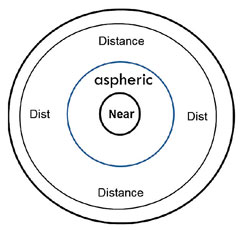
Instituting these concepts into practice can help develop a systematic approach for multifocal selection and can help you make any necessary modifications to the lens. Gathering the patient’s refraction values, photopic and scotopic pupil size measurements and their near and distance visual requirements can assist with solidifying the initial parameters for the lens. Addressing the lens prescription typically follows a simple rule: patient’s requiring smaller adds generally perform better with distance-centered lens designs. In this case, line of sight will have a minimal effect and pupil size will likely be larger. The spread function of powers through a low add power aspheric multifocal design is also less compressed than high power adds, so the pupil will, for the most part, have the space to capture the near prescription powers. Higher add prescriptions, however, are more likely to perform successfully in near-center designs due to the add power spread function compression. With this design, smaller pupils will result in improved distance vision as it dilates under scotopic conditions (Figure 3).
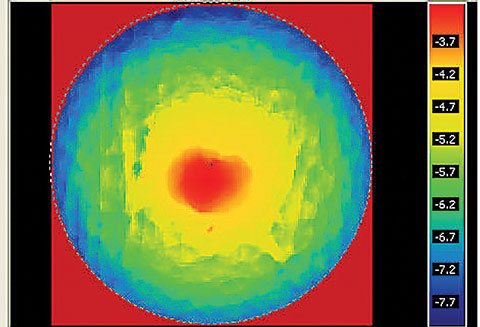 |
| Fig. 3. A contact lens near-center power profile. |
Customization
Tailoring a multifocal lens design to the patient’s needs plays an important role when the necessary parameters are not available in stock multifocal lens designs. Setting specific zone size configurations and decentering optics to position line of sight are important tools in ensuring multifocal lens success.
Customized lenses can also help with reduced contrast sensitivity, coma, astigmatism and ghosting, which are some of the optical reasons patients complain of poor vision through multifocal lenses.
When conversing with the patient regarding their specific visual needs, it is important to determine whether they are near-centric or distance-centric. To achieve this, the common practice is to display the Snellen chart to the patient and ask them which lines they can see clearly. Though the chart is needed, the real analysis should occur when the patient goes home and performs at work, where they can assess whether the lenses are suitable or further modifications are necessary in different environments.
Selecting the Design
The same philosophies hold true whether the patient is wearing soft, hybrid or gas permeable multifocal contact lenses. Hybrid, scleral and soft lenses tend to move minimally on the eye with blinking, while rigid corneal gas permeable lenses move vertically. Because intermediate vision is an important zone for most patients today with the pervasive use of computers and cell phones in daily life, concentric designs have fallen out of favor in deference to aspheric ones. Concentric lens designs still have use when the patient’s accommodative facility remains active enough to trigger intermediate vision. However, in cases in which higher add prescriptions are necessary, the only configuration that will work successfully is modified monovision.
Hybrid multifocal contact lenses can be fabricated in both a concentric and aspheric progressive lens design. The concentric stock zone parameter is typically configured in a 1.9mm or 2.2mm near-center design, while the aspheric lens design has a 3.0mm near-center aspheric lens design. The advantage of these multifocal lens designs is that the lens configurations center extremely well; however, the fact that the near center zones are fixed can be a problem. In order to improve the patient’s visual success, you can modify the optical zones in both bifocal and multifocal lens designs: For example, as the center zone increases in size, it has a negative effect on the surrounding area, while if the surrounding area increases in size, then it has a negative effect on the center area (Figure 4).
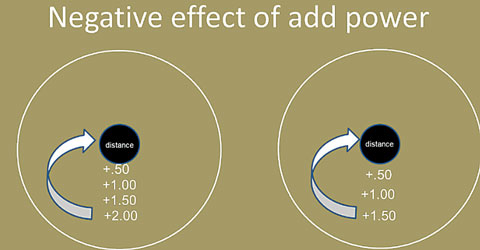 |
| Fig. 4. Negative impact of near surround zone affecting distance-center lens zone. Increasing the strength of the add increases the strength of the impact. |
Severe dry eye patients, such as those who suffer from Sjögren’s syndrome, graft-vs-host disease or Stevens-Johnson syndrome, may benefit from scleral multifocal contact lens wear, as the lens vaults the cornea to land on the sclera and contains a fluid-filled compartment to assist with corneal surface hydration. These lenses are also suitable for patients with keratoconus or other corneal irregularities. This is especially the case since a scleral lens design can be customized and tailored to fit the patient’s unique pupil size and corneal configuration.
For most patients, following assessment of pupil size under photopic and scotopic conditions using the Volk eye check, ruler or pupillometer, the lens design should be configured in either an aspheric or concentric lens design. Note, the most successful design configuration for these patients may be a near aspherical zone, surrounded by an aspheric zone and then a spherical distance zone: a patient requiring an oblate design with a 3.3mm photopic pupil and 4.1mm scotopic pupil would ultimately end up with a lens comprised of a 1.8mm near central spherical zone and a 1.2 aspheric zone, with the distance zone starting at 3.0mm extending out to 8.0mm, or the size of the total optic zone (Figure 5).
 |
| Fig. 5. A common multifocal design (spherical near aspheric intermediate and spherical periphery distance). |
Scleral lens designs also allow for decentered optics to be ordered, which can help neutralize line of sight offsets. The inclusion of quadrant specific peripheral curves is an additional option that may help provide better centration.
Multifocal soft lenses are available in daily, monthly and quarterly as well as yearly replacement schedules, while lens designs can be fabricated in near-center, distance-center, aspheric, concentric and combination options. Soft multifocal lenses generally contain fixed zone size parameters, regardless of the wearer’s pupil size or line of sight, which can lead to a trial and error approach for fitting. Customized soft multifocal lenses are able to be fabricated in any zone size, diameter, base curve and also with decentered optics to neutralize offsets of line of sight. Regardless, however, soft multifocal lenses provide a good option for simultaneous vision due to their restricted movement on the eye during blink.
Use of a multifocal simulator may be a good starting point when determining the lens’s zone size configuration, as it specifies either a near center design or distance center design (Figure 6). Furthermore, in the simulator, the add power will provide the visual outcome relationship between distance, intermediate and near.
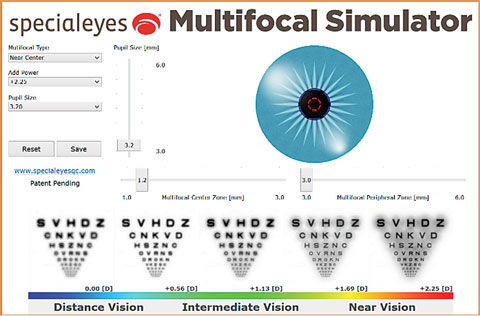 |
| Fig. 6. Multifocal Simulator. Variables include pupil size, add power, zone size, distance-center or near-center design. |
The resultant visual acuity is represented by a series of Snellen acuities across the entire visual range. The multifocal simulator also illustrates the fact that when add power increases, contrast sensitivity decreases; it also demonstrates the resultant visual acuity in cases when the pupil size or add changes, without the need to place a lens on the eye. Simulation can also help portray the difference between the resultant acuity in cases when a near-center lens is employed, as opposed to a distance-centered lens.
Rigid GPs
Corneal gas permeable multifocal lenses are an additional lens design that can be considered by presbyopic patients. Unlike hybrid, scleral and hydrophilic lenses, corneal GPs move on the eye—a unique characteristic that enables the lens to translate on the ocular surface itself, enabling the eye to move vertically through the lens upon downward gaze to reach the add power. Centering the lens in front of the pupil can be achieved via altering the lift of the lens. Because corneal GP lenses float on a layer of tears, controlling the tear layer will lead the lens to ride either higher or lower on the eye. This can done either by changing the lens’s base curve, or by altering the diameter of the lens. As such, when the tear layer becomes deficient or changes during wearing time, visual acuity can be compromised due to adjustments in lens movement and lift, which affects lens position on the eye.
As stated earlier, pupil size is the controlling factor of every multifocal design, and corneal GP lenses are no exception to this concept. Corneal GP multifocal optics are most commonly adjusted by changing the eccentricity of the lens design. Pupil size and near power requirements determine the rate of flatting throughout the optics of a GP lens: for example, a larger pupil can capture more of the peripheral zone than a smaller pupil (Figure 7). A small pupil will also need a more rapid power change through the optics of the lens to reach the peripheral zone prescription. Furthermore, smaller adds require less lens power change, while larger add powers require a more significant power change. Power compression in the case of aspheric lens designs is controlled through eccentricity: by measuring pupil size, eccentricity can be prescribed to enhance both distance and near vision. Overall, success with aspheric multifocal lenses can be achieved via control of lens placement on the eye. This is accomplished by adjusting lift and power requirements, which are associated with eccentricity defined by pupil zone.
 |
| Fig. 7. Reduced center-near zone to change aspheric power compression. |
While the options for multifocal contact lenses are more numerous than ever before, the presbyopic population still, for the most part, remains underserved. Though dry eye syndrome is one major cause of contact lens dropout, requiring patients to wear reading glasses in addition to their contact lenses can frustrate many of them and cause them to forgo contact lenses entirely. Constructing a multifocal contact lens design in which the line of sight transcends into the refractive add power while avoiding the degradation of distance acuity can help increase interest in multifocal lenses.
The making of zone size modifications related to pupil size is another way to boost product visibility and patient satisfaction, while base curve, diameter, power, pupil size, eccentricity and near-center or distance-center lens designs are the key parameters to select for to improve the prescription of multifocal contact lenses.
Above all, however, a final frontier exists in improving patient comfort in this population. Ultimately, material enhancements will prove the source of the greatest comfort during wear for all of the multifocal contact lens patients we see in the clinic.
Dr. Davis practices in Oak Lawn, Ill. He is a cofounder of EyeVis Eye and Vision Research Institute, where he develops contact lens designs and anterior segment pathophysiology research. Dr. Davis is an inductee in the National Academy Practice in Optometry and is an advisor to the Gas Permeable Lens Institute. He has also been honored as one of the 50 most influential optometrists in 2015.
