Bright Ideas for Better ExamsThe February 2023 issue of Review of Optometry is our annual diagnostic skills and techniques issue. In each article, eyecare experts offer practical tips and advice to help you brush up on exam techniques that you can put to use everyday in your office. Check out the other articles featured in this issue:
|
As you’re reading through these suggestions, keep in mind the words of Oliver Sacks: “There is only one cardinal rule: one must always listen to the patient.”2
 |
|
Fig. 1. Dr. Tyler taking a patient’s case history. |
Intake Forms
To gather a more efficient and comprehensive case history, clinicians should first consider the type of intake forms given to their patients. These documents are available in a wide variety of styles depending on the practitioner’s preferences and goals. Often, offices incorporate a generic intake form, whether on paper or within an automated system, that does not reflect the clinic’s environment or demographics. On the other hand, when these forms do reflect the type of practice, doctor’s specialty and common patient populations seen within the office, the information collected will enhance the quality and efficiency of the case history and exam. An example of this customization could be adding keratoconus as a pertinent part of an ocular history intake form at a specialty contact lens practice.
We provided an example of an intake form that you can download here and throughout this article we’ll highlight different sections that can be modified to better suit the needs of your patients. This involves taking into consideration factors such as demographics and commonly treated conditions at your clinic, as well as your practice modality. Taking the time to customize these tools for your office will guide the case history interview and allow you to recognize earlier in the exam the types of conditions you may be looking for. Consider tearing out the example intake form to use at your practice or reference when contriving your own.
Ensure inclusivity. Intake forms with inclusive language can set the tone for a patient’s experience in the office and help establish trust even prior to being seen by a technician or the doctor. Options for pronouns with checkboxes and a “fill-in-the-blank” line allow patients to easily select how they identify themselves. While we often use “other” in various portions of our intake forms (e.g., “other medications”), the use of “other” in the setting of pronouns can alienate patients who don’t fit into the listed categories.3 By including an option to write in pronouns that aren’t listed, the practice indirectly supports inclusivity (see the following example).
Example of demographic collection with attention to inclusivity:
Chosen Name (Last, First): __________________________________________
Legal Name (if different from chosen): _________________________________
Date of Birth: ________ Birth sex: ____ Pronouns: X he/him X she/her
X they/them X _______________
Address: _______________________________
City: ________________________
State: ____ Zip: ________
Home Phone: _________________
Cell Phone: ___________________
Ask patients directly about past cosmetic procedures. When completing an intake form or during case history, many patients may not think to disclose past facial cosmetic procedures such as Botox or blepharoplasty. Some might be hesitant to admit it and others may not realize it’s germane to eye health. Here’s why they’re mistaken.
Botulinum toxin belongs to a class of medications described as neurotoxins and is used for the management and treatment of both therapeutic and aesthetic applications. Therapeutic uses for botulinum toxin (Botox) include chronic migraines, musculo-spasmodic disorders (such as blepharospasm and hemifacial spasm), occipital or trigeminal neuralgia and numerous other systemic spasmodic and pain associated conditions—in addition to use for cosmetic purposes.4
While patients may not think to associate recent Botox injections or other cosmetic procedures with visual symptoms such as new-onset diplopia, facial paresis or symptoms of dry eye, aesthetic procedures have been shown to result in ocular complications.5-7 Some examples of specific complications from elective cosmetic surgery include periocular botulinum toxin injection that may result in decreased tear expression due to infiltration of the lacrimal gland and dermal fillers that have been associated with retinal arterial occlusions, causing temporary or even permanent vision loss.5,6
Additionally, even if an outcome is cosmetically “successful,” the procedure may result in restrictions to lid-closure strength associated with Botox or overcorrection on blepharoplasty that can cause exposure-related dry eye.
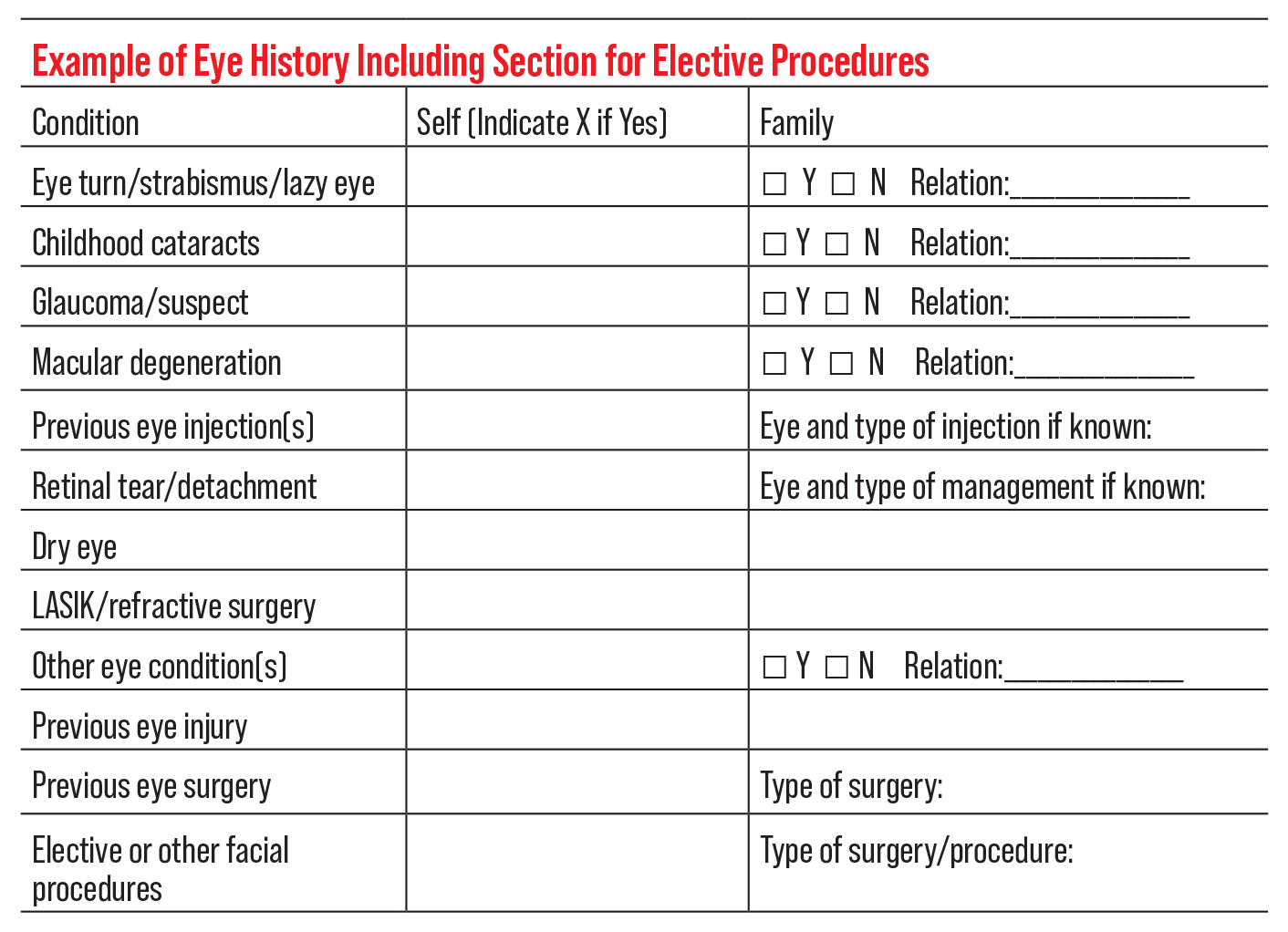 |
| Click image to enlarge. |
For all these reasons, creating space on the intake form—or including questions within your verbal case history—to ask patients specifically about elective/cosmetic procedures may be invaluable to identifying potential etiologies and addressing their visual symptoms while helping streamline the exam (see example above).
Be mindful of patients using high-risk medications. In addition to the medications prescribed by optometrists, there are a wide variety of drugs that can have ocular side effects or adverse reactions (Table 1).8,9 Ideally, the risks should be identified early in an exam to guide the practitioner’s attention during the ocular health evaluation and to identify necessary ancillary testing. Ocular risks from pharmaceutical agents may result from any formulation of a medication (e.g., topical, oral, inhaled) although some presentations may have higher risk of side effects. Specifically inquiring within the intake and/or early in the verbal case history about the use of OTC medications, topical agents (e.g., creams, gels, ointments) and inhalers may allow practitioners to identify potential complications and ocular impacts of these less commonly reported methods of medication distribution.
In an observational case series comparing self-reported medication use from patients at follow-up visits in a primary care clinic with their EMR prescription orders, upon reconciliation almost 75% of patients had at least one discrepancy in medication, dosing or frequency. The most common type of discrepancy was an incorrect medication documented in the chart, and most were related to OTC use.10
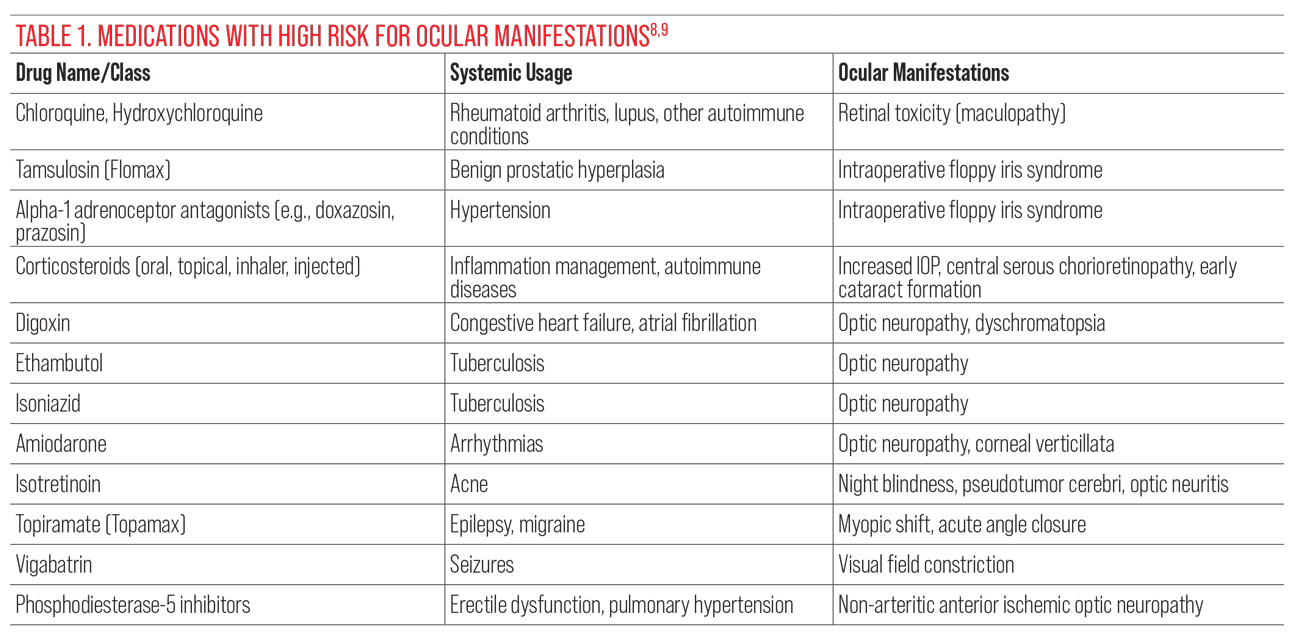 |
| Click image to enlarge. |
When ocular complications/side effects occur, they range from mild to severe, asymptomatic to symptomatic, including risks for significant vision loss. Table 1 lists medications with ocular risks, including those more commonly encountered medications with potentially serious ocular adverse events and ones to be attentive to when reviewing your patients’ medication history.
Two medications that are commonly prescribed and associated with significant ocular risks in which we play a role in decreasing potential complications are tamsulosin (Flomax) and hydroxychloroquine (Plaquenil). These may warrant specific inquiry on an intake form or within a case history interview to ensure proper additional testing is completed and risks are communicated to the patient’s providers for best interprofessional collaborative care and prevention (see example below).
Example of specific medication inquiry for ocular risk management:
Are you currently on or have you previously taken either of the following medications:
Tamsulosin (Flomax)
X YES X NO
Hydroxychloroquine (Plaquenil)
X YES X NO
If Yes, current dose: _______________ current weight: _____________
A known history of tamsulosin use is critical for patients planning to have cataract extraction, as any prior use can lead to intraoperative floppy iris syndrome.11 Discontinuation of tamsulosin prior to surgery may decrease but not eliminate the risk for the condition, partially due to the drug’s long half-life. Tamsulosin can also irreversibly block a-1 adrenoceptors, potentially resulting in permanent iris atrophy. While some risks during cataract surgery may persist, noting other patient-related risk factors (including other risk-associated medications) and taking the appropriate pre- and intraoperative measures can address and/or prepare for potential cataract extraction complications and decrease overall risk for the patient.12
While the mechanism of hydroxychloroquine toxicity is not fully understood (or, for that matter, the medication’s ability to support patients with a variety of autoimmune disorders), its potential for retinopathy is well-established and may be a reason that patients are referred to your practice for baseline examinations and ongoing monitoring of ocular risks. The guidelines for monitoring patients using hydroxychloroquine have been updated several times, with the most recent (as of this writing) being from 2016.13 Management guidelines rely on additional personal information about the patient, including their dosing of mg/kg/day and medication use duration. If your practice frequently sees patients with rheumatologic conditions using hydroxychloroquine, a dedicated space for additional patient information—such as current dosage, length of use and body weight—on an intake form is ideal for making risk assessment easier to calculate.
Ask about past COVID-19 infection. Although COVID symptom screenings have very much been on the forefront of our intake processes since 2020, inquiring about date(s) of infection and symptoms of “long COVID” may be a less customary practice. Beyond follicular conjunctivitis, COVID-19 infections can result in ocular manifestations such as cotton wool spots and retinal hemorrhages, retinal vascular occlusions, optic neuritis and paracentral acute middle maculopathy.14,15 Additionally, the medical community does not understand the long-term ocular risks of COVID-19 infection. Specifically including past infection with COVID-19 within the medical history review may be beneficial in determining a potential etiology for ocular findings in a patient that does not fit a more established or other disease-related profile.
 |
| Fig. 2. This case of red eye in a patient presenting for a problem-focused exam may require fuller analysis of review of systems and questioning about STI. Click image to enlarge. |
Now that we’ve discussed what to include and be mindful of on patient intake forms, let’s review how to continue forming a sensible case history during the clinical examination.
EHR Systems and Record-Keeping
While there certainly are benefits to creating a readable template of data within an electronic health record (EHR) system, the EHR format may not be the most conducive to an efficient and personalized case history. The standard template design might make it challenging to understand each patient’s needs and create a flow of questions that allows the clinician to fully appreciate the patient’s health narrative. EHR templates are designed to fit within a screen and thus, often are not ideal for the actual nature of interviewing the patient in the exam chair.
In a study from 2015 regarding a qualitative assessment of EHR and “building the patient’s story,” the data revealed that EHR was obstructive to a clinician’s ability to fully build the patient’s story due to fragmentation of data and limits to the number and size of free-text spaces available for notes.16 In short, the constraints of the EHR system “inhibited the clinicians’ ability to read the why and how interpretations of clinical activities,” especially if the care involved multiple team members. Varpio et al noted that EHR systems negatively impacted clinical reasoning and interprofessional collaborative practices, taking a longer time to “build the patient’s story.”16
For the reasons outlined, creating supplementary methods of assessment (e.g., customized/localized intake forms, symptom surveys) and incorporating practices, like those listed below, may compensate for the limitations of an EHR case history template.
Whether you plan to record case history within an EHR or supplementary system, below are a few guidelines on best practices to optimize documentation of patient data.
Don’t fall victim to “copy and paste.” Now that most medical offices rely on electronic record-keeping, it can be tempting to cut corners for the sake of time, such as copy-forwarding the records of a patient’s previous visit without edits. The practice of “copy and paste” is dangerous, as it discourages accurate updating of case histories, medications and potentially other exam components. When not edited, this shortcut omits patients’ personal updates on their own health and well-being. Documenting how patients feel in their own words is an essential part of ongoing care, as it helps provide a fuller picture of the signs and symptoms, they experience from one visit to the next. As a reminder, Table 2 lists best practices for EHR documentation as suggested by Weis and Levy.17
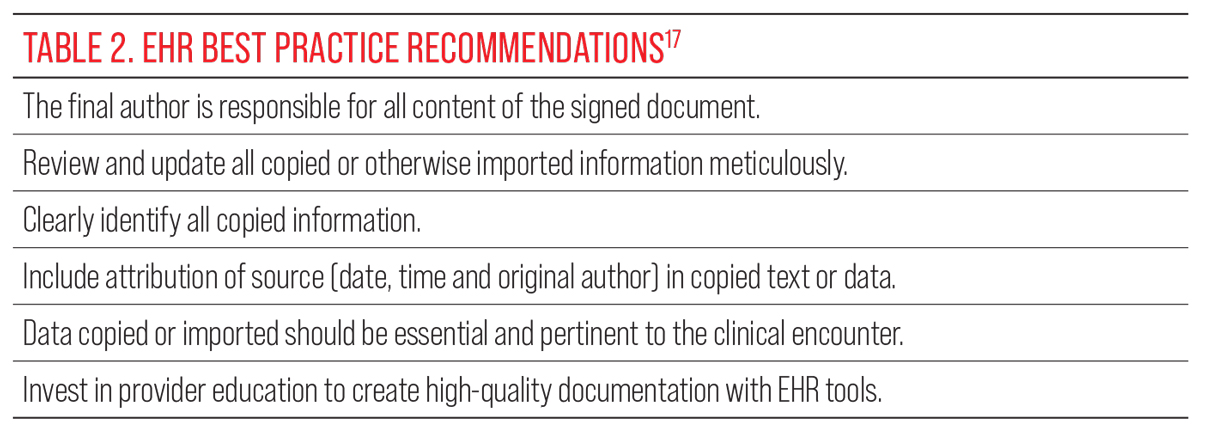 |
| Click image to enlarge. |
Be mindful of proper abbreviation use. The Institute for Safe Medicine Practices (ISMP) publishes the ISMP List of Error-Prone Abbreviations, Symbols and Dose Designations.18 This list contains various abbreviations, symbols and dose designations that have been found in medical records and/or prescriptions and were reported through the ISMP National Medication Errors Reporting Program as associated with harmful or potentially harmful medication errors. It’s recommended that these abbreviations/symbols never be used in medical communication. The list also identifies abbreviations/symbols that the Joint Commission recognizes on its own “do not use” list. Unfortunately, this list does contain the commonly used ocular abbreviations of OD and OS for right eye and left eye, respectively, as they can be confused with AD and AS (right ear, left ear). While unlikely to confuse eyecare providers, other healthcare practitioners may confuse the ocular and auditory abbreviations. Within an interdisciplinary setting, and when records may be seen by other types of healthcare providers, it is best to avoid the abbreviations OD and OS, as well as the other abbreviations/symbols on the ISMP list.
Asking Difficult Questions
Another area that can complicate taking patient histories during the exam involves discussing issues that may be perceived as sensitive topics from a patient perspective. Issues that are traditionally private—such as last menstrual period, sexual activity and mental health status—may be important to inquire about for the care of our patients. Not only may they be surprised that their eye doctor is interested in these areas of medical history, but patients may also not be forthright in disclosing information due to societal “norms” and expectations. Nevertheless, these personal history components may be crucial to determining differential diagnoses and related conditions, and what to prescribe for therapeutic management.
Let’s discuss how to best communicate topics that may be sensitive to some patients.
Pronouns. While asking patients which pronouns they use might initially seem awkward, using the wrong ones is an even bigger blunder. Using correct pronouns throughout the examination and case history demonstrates respect and inclusivity, and consequently, it can help build patient rapport. Patients may not disclose pertinent information if they feel alienated at any point during the appointment.19 On the other hand, some patients are unaccustomed to these types of questions and may react adversely to them. How do we balance this?
This is where intake forms and annual history updates can be beneficial, recognizing that gender identity may change over time. Normalizing gender identity throughout the office can be helpful to create a safe space. For example, using pronoun identification on staff and doctor nametags and introductions such as, “Hello, my name is Dr. Eye. My pronouns are she/her. How would you like to be addressed?” can reinforce positive attitudes and patient commitment to the practice.20
Substance use. Inclusion of social history questions regarding substance use on a patient response intake form may help break the ice for conversations regarding use of alcohol, tobacco, vaping and other legal and/or illegal drugs. Substances that are subject to abuse can affect the eye either directly (e.g., alcohol-induced diseases such as optic neuropathy) or indirectly (e.g., talc retinopathy associated with cocaine use).21-22 Eloge et al has proposed incorporating questions regarding substance use into the history of present illness rather than only in the social history due to the fact that substance use disorders are pervasive in the US and permeate a variety of medical specialties.23 Explaining the reasoning behind the case history questions can help reassure patients of your goals for inquiry and provide them with a more complete understanding of various factors that connect to ocular health.
In the current age of EHRs and patient portals, patients may want access to their exam records. While they may use colloquial language to describe their substance use, the use of person-first language by healthcare professionals is critical in reducing stigma around substance use disorders. For example, instead of documenting “patient is a substance abuser,” an alternative would be, “patient has a history of substance use disorder” or “patient who uses IV drugs.”24
Sexually transmitted infections (STIs). The CDC has excellent resources about STIs, including “A Guide to Taking a Sexual History.”24 Within the recommendations for taking STI history is a suggestion to follow what’s known as the “5 Ps” approach, representing questioning of the patient regarding (1) Partners, (2) Practices, (3) Protection from STIs, (4) Past history of STIs and (5) Pregnancy intention. A deeper dive into case history, including STI inquiry, may be warranted in situations when patients come for an exam with an atypical red eye (e.g., hyperacute conjunctivitis) or persistent red eye despite attempted management or when traditional questions regarding discharge and exposure to another person with a red eye are unclear (Figure 2). In such cases, careful review of the patient’s review of systems in the areas of genitourinary symptoms, rashes and feelings of general fatigue and/or malaise may suggest or support questioning regarding recent sexual activity, understanding that the patient may require additional workup including an assessment for STI.
The patient may be guarded in their response to these types of questions; however, educating them as to why you’re performing a more complete case history may encourage understanding and openness on their part. Also, if STI testing is recommended based on history, having a list of patient resources in your area is essential.
Continuing History Post-Exam
Forming a complete case history for each patient takes place before an exam via intake documents, at the start of an exam with a formal history interview and during the exam as concerning clinical findings are identified and warrant questioning. Case history may also continue during downtime (e.g., dilation) or beyond the allotted exam time by utilizing various surveys and questionnaires. These ancillary tools are especially valuable for patients with findings that warrant timely follow-up, additional management/comanagement and those suffering from conditions that have been previously studied and assessed (Table 3). Examples of conditions with well-established and validated surveys and questionnaires include dry eye, convergence insufficiency and uveitis, to name a few.
Table 3. Standardized History Surveys | ||||
Ocular Diseases |
| |||
MERSI: Ocular Inflammatory Disease Review of Systems25 |
| |||
Dry Eye | ||||
Standard Patient Evaluation of Eye Dryness Questionnaire (SPEED)26 |
| |||
Ocular Surface Disease Index (OSDI)27 | | |||
Binocular Vision | ||||
Convergence Insufficiency Symptoms Survey (CISS)28 |
| |||
Diplopia Questionnaire29 |
| |||
Having printed copies of questionnaires for patients to fill out during downtime may be an effective use of in-office time. However, these surveys, especially those that are longer, can also be provided to patients to fill out at home prior to their next visit. This allows the patient to gather additional history and reflect about ongoing signs and symptoms prior to their follow-up visit, which may help further direct long-term care. This type of “continued” case history may also be used for patients who do not have a definitive diagnosis but have findings warranting additional workup such as in the case of a new, bilateral uveitis patient or patients who have variable symptoms (Figure 3).
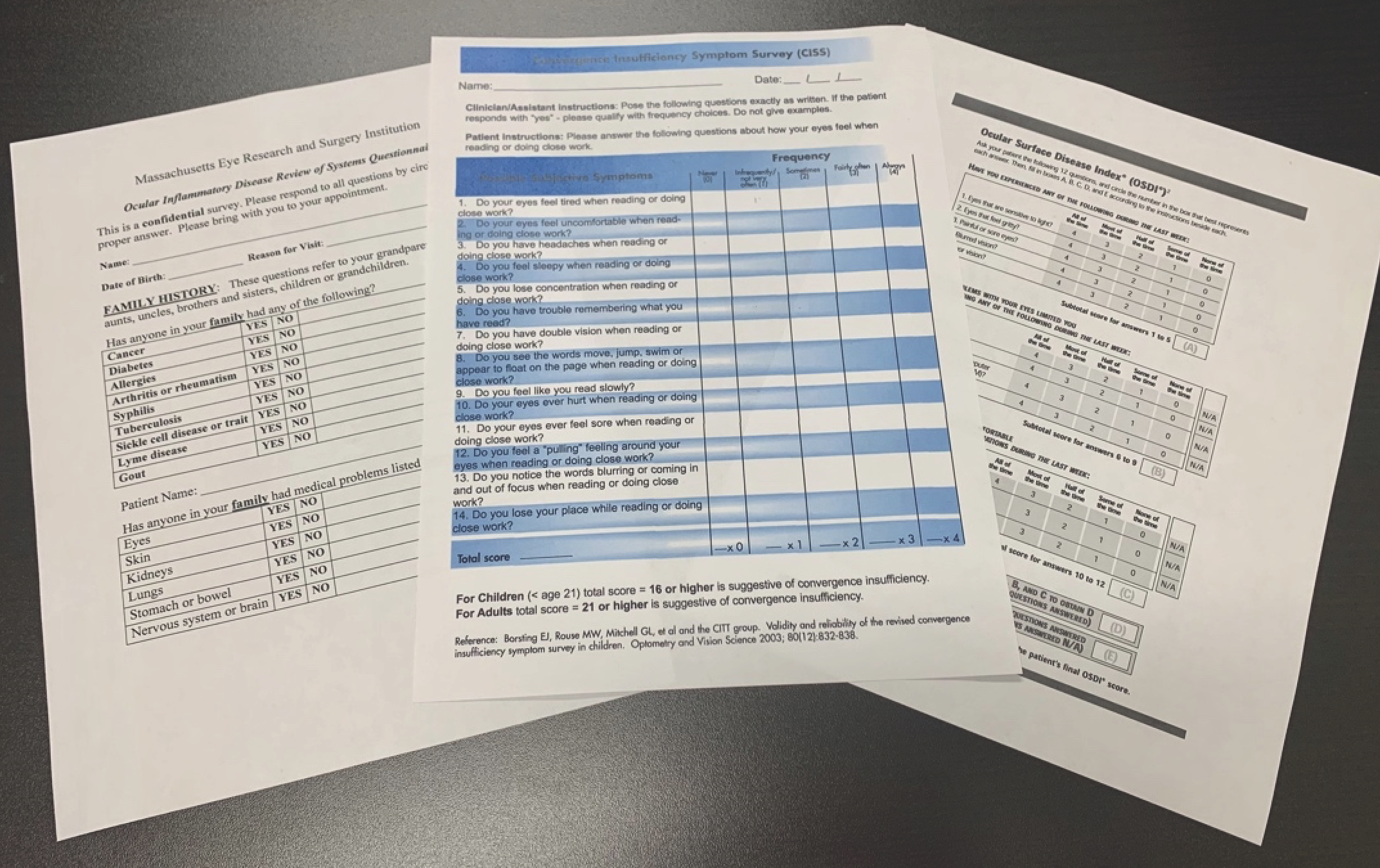 |
| Fig. 3. Various standardized surveys, which may be printed out for patients with specific ocular findings to assist in more complex histories before or after an exam. (Left to right: MERSI, CISS, OSDI). Click image to enlarge. |
As suggested for patient intake forms, it may also be helpful to find surveys and questionnaires that reflect the type of patients most frequently seen at your practice. For example, if you work at a low vision practice, you may want to include night blindness as a question on the patient history form.
A resource available to the public for various standardized tests in the areas of pediatric and binocular vision management—including surveys of symptoms related to atropine for myopia and nasal-lacrimal duct obstruction—may be found at: public.jaeb.org/pedig/view/reference (associated with the Pediatric Eye Disease Investigator Group). Dry eye questionnaires and surveys have been curated by EyeWiki and can be downloaded at: eyewiki.aao.org/dry_eye_syndrome_questionnaires.
Final Thoughts
Case history information gathered by a variety of methods can guide and direct patient examinations. Efforts to adapt intake forms and history-taking techniques to reflect a practice’s community may be invaluable to provide effective patient care.
We’ll leave you with a few insightful words from Warner Slack, MD, an EHR pioneer: “The largest and least utilized healthcare resource is the patient him/herself.”31
Dr. Tyler is an associate professor at Southern California College of Optometry at Marshall B. Ketchum University. Dr. Tawa is currently on faculty at Southern California College of Optometry at Marshall B. Ketchum University. They have no financial interests to disclose.
1. Halkett GKB, McKay J, Shaw T. Improving students’ confidence levels in communicating with patients and introducing students to the importance of history taking. Radiography. 2011;17(1):55-60. 2. Oliver Sacks (2013). “Migraine”, p.309, Vintage from Oliver Sacks. (n.d.). AZQuotes.com. www.azquotes.com/quote/827371. Accessed December 12, 2022. 3. Kronk CA, Everhart AR, Ashley F, et al. Transgender data collection in the electronic health record: current concepts and issues. J Am Med Info Assoc. 2011;29(2):271-84. 4. Busey B, Esparza MJ. The evidence for noncosmetic uses of botulinum toxin. J Fam Pract. 2020;69(9):447-53. 5. Coroneo MT, Rosenberg ML, Cheung LM. Ocular effects of cosmetic products and procedures. Ocul Surf. 2006;4(2):94-102. 6. Ricci LH, Navajas SV, Carneiro PR, Söderberg SA, Ferraz CA. Ocular adverse effects after facial cosmetic procedures: a review of case reports. J Cos Derm. 2015;14(2):145-51. 7. Langsdon PR, Schroeder RJ 2nd. Recognizing, managing, and guiding the patient through complications in facial plastic surgery. Facial Plast Surg Clin North Am. 2020;28(4):483-91. 8. Pula JH, Kao AM, Kattah JC. Neuro-ophthalmologic side-effects of systemic medications. Curr Opin Ophthalmol. 2013;24(6):540-9. 9. Syed MF, Rehmani A, Yang M. Ocular side effects of common systemic medications and systemic side effects of ocular medications. Med Clin North Am. 2021;105(3):425-44. 10. Stewart AL, Lynch KJ. Identifying discrepancies in electronic medical records through pharmacist medication reconciliation. J Am Pharm Assoc. 2012;52(1):59-68. 11. Christou CD, Tsinopoulos I, Ziakas N, Tzamalis A. Intraoperative floppy iris syndrome: updated perspectives. Clin Ophthalmol (Auckland, NZ). 2020;14:463. 12. Kumar A, Raj A. Intraoperative floppy iris syndrome: an updated review of literature. Int Ophthalmol. 2021;41:3539-46. 13. Marmor MF, Kellner U, Lai TY, Melles RB, Mieler WF. Recommendations on screening for chloroquine and hydroxychloroquine retinopathy (2016 rev). Ophthalmol. 2016;123(6):1386-94. 14. Sen M, Honavar SG, Sharma N, Sachdev MS. COVID-19 and eye: a review of ophthalmic manifestations of COVID-19. Indian J Ophthalmol. 2021;69(3):488. 15. Zhang Y, Stewart JM. Retinal and choroidal manifestations of COVID-19. Curr Opin Ophthalmol. 2021;32(6):536-40. 16. Varpio L, Rashotte J, Day K, King J, Kuziemsky C, Parush A. The EHR and building the patient’s story: A qualitative investigation of how EHR use obstructs a vital clinical activity. Int J Med Inform. 2015;84(12):1019-28. 17. Weis JM, Levy PC. Copy, paste, and cloned notes in electronic health records. Chest. 2014;145(3):632-8. 18. Institute for Safe Medication Practices (ISMP). ISMP list of error-prone abbreviations, symbols, and dose designations. ISMP. 2021. 19. Bindman J, Ngo A, Zamudio-Haas S, Sevelius J. Health care experiences of patients with nonbinary gender identities. Transgender Health. 2022;7(5):423-9. 20. The Washington Post. The inclusivity trap. Published February 9, 2021. www.washingtonpost.com/outlook/2021/02/19/gender-pronouns-doctors-patients-medical. Accessed December 2022. 21. Karimi S, Arabi A, Shahraki T. Alcohol and the eye. J Ophthalmic Vis Res. 2021;29;16(2):260-70. 22. Shah VA, Cassell M, Poulose A, Sabates NR. Talc retinopathy. Ophthalmology. 2008;115(4):755. 23. Eloge J, Napier TC, Dantz B. Integrating substance use disorders or “use” into the medical history. Sub Abuse. 2018;39(4):505-8. 24. Chan C. Back to basics: a stigma-free history. The Curbsiders. thecurbsiders.com/addiction-medicine-podcast/8-back-to-basics-a-stigma-free-history. Accessed December 2022. 25. Centers for Disease Control and Prevention. A guide to taking a sexual history. 2021. www.cdc.gov/std/treatment/sexualhistory.htm. Accessed December 2022. 26. Foster CS, Vitale AT. Diagnosis and treatment of uveitis. 2nd ed. New Delhi: Jaypee Brothers Med Pub Ltd. 2013;20-32. 27. Ngo W, Situ P, Keir N, et al. Psychometric properties and validation of the standard patient evaluation of eye dryness questionnaire. Cornea. 2013;32(9):1204-10. 28. Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 2000;118(5):615-21. 29. Convergence Insufficiency Treatment Trial (CITT) Investigator Group. Validity of the convergence insufficiency symptom survey: a confirmatory study. Optom Vis Sci. 2009;86(4):357. 30. Holmes JM, Liebermann L, Hatt SR, Smith SJ, Leske DA. Quantifying diplopia with a questionnaire. Ophthalmology. 2013;120(7):1492-6. 31. deBronkhart D, Sands DZ. Warner Slack: patients are the most underused resource. BMJ. 2018;362:k3194. |