 |
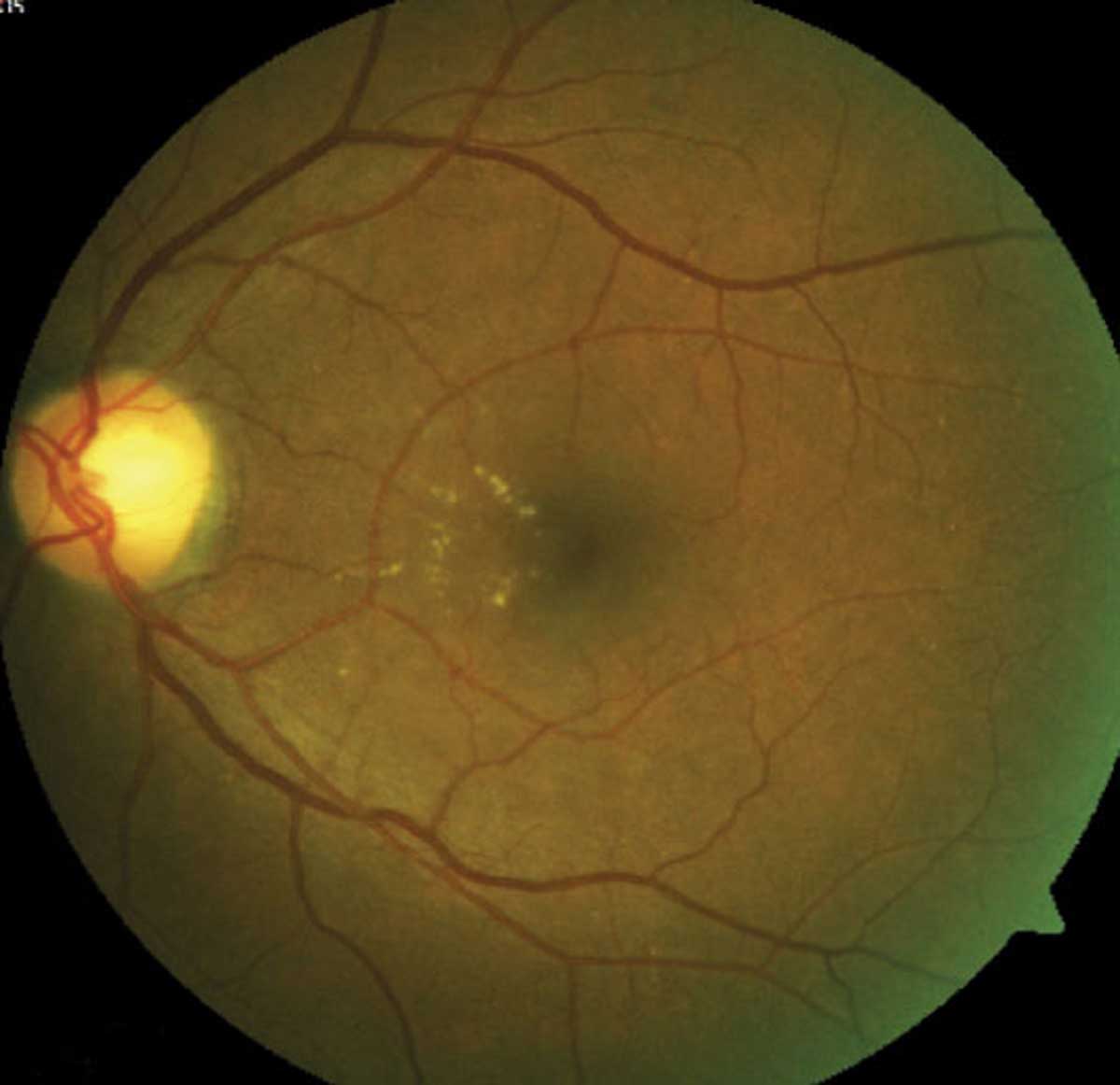
No correlation between DME development and DR severity was found in this study. Click image to enlarge. |
To better understand diabetic macular edema’s (DME) progression and determine more timely, targeted treatments in the initial stages of nonproliferative diabetic retinopathy (NPDR), researchers followed 74 patients for three years and studied the rates of occurrence of DME.
OCT, OCT-A and OCT leakage were used to examine eyes in the initial stages of NPDR, identified by the Early Treatment Diabetic Retinopathy Study (ETDRS) grading scale (10-47). Retinal edema was measured with central retinal thickness and retinal fluid by using optical reflectivity ratios obtained with the OCT leakage algorithm, and vessel density was measured on OCT-A.
DME was identified during the first visit in 9% of eyes with ETDRS ratings of 10 to 20, 10% of eyes with a rating of 35 and 15% of eyes with ratings of 43 to 47.
“In summary, subclinical DME can occur very early in the disease process and, in general, is not apparently related to DR severity,” the study authors concluded.
Neither subclinical or clinical DME showed significant progression or an association with retinopathy severity worsening, but affected eyes did show an increase in retinal extracellular fluid during the three-year follow-up and had a higher risk of vision loss.
“It is apparent from this study that subclinical DME does not inexorably progress over time scales of one to three years, and, furthermore, a fraction of these eyes spontaneously improved,” the authors explained. “We observed, however, in the three-year period of follow-up, that some eyes with increased central retinal thickness show a progressive increase in low optical reflectivity values, indicating a progressive increase in retinal extracellular fluid accumulation when there is a chronic and prolonged situation of increased retinal thickness, representing edema.”
“Furthermore, eyes with DME and visual loss show a clear association with increased retinal fluid accumulation, demonstrated by increased low optical reflectivity ratio values, whereas eyes with DME and no vision loss did not show increases in extracellular retinal fluid,” they continued. “Abnormal accumulation of retinal extracellular fluid appears to be a good indicator for the need for close monitoring with potential for early treatment. Further investigations such as fundus fluorescein angiography may be utilized to assess the ischemic element of macular edema.”
Lobo C, Santos T, Margues IP, et al. Characterization of progression of macular edema in the initial stages of diabetic retinopathy: a three-year longitudinal study. Eye. January 22, 2022. [Epub ahead of print]. |

