 |
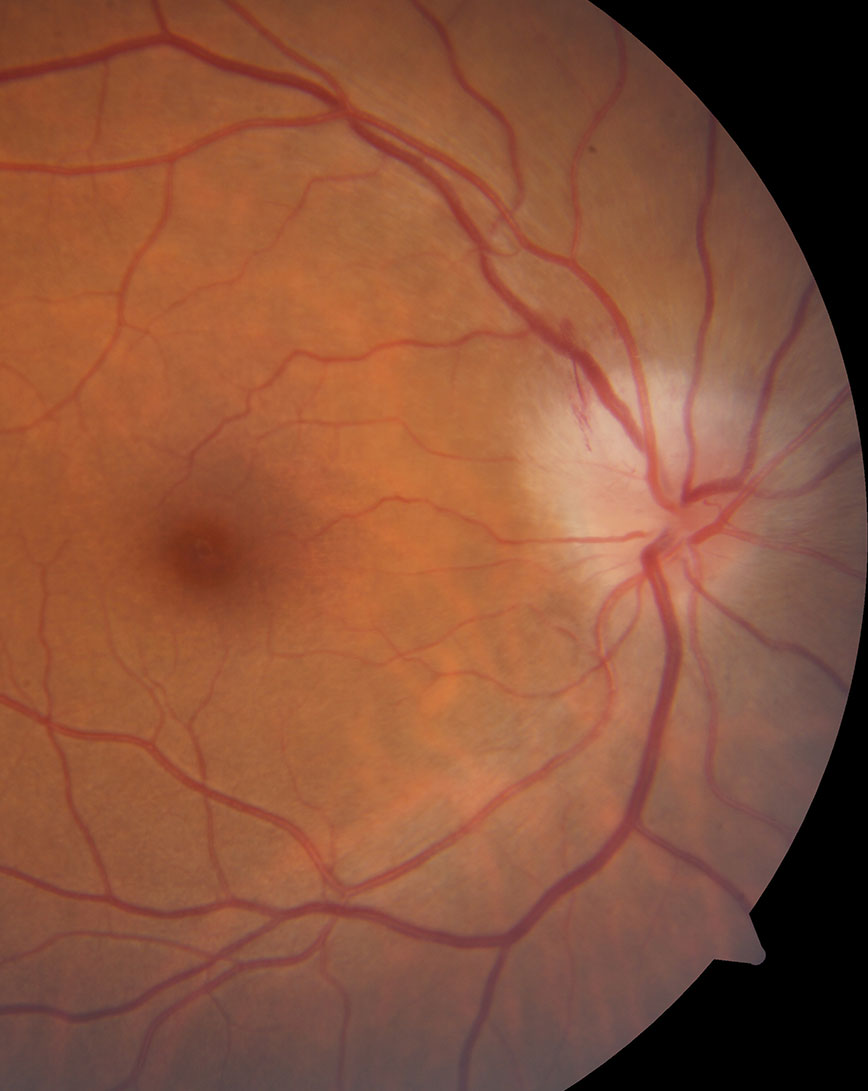
| Creating hospital protocols for neuro-ophthalmologic conditions like TIA-related transient vision loss, acute central retinal artery occlusion, papilledema and optic neuritis (pictured) could streamline management of complex patients. Photo: Nate Lighthizer, OD. Click image to enlarge. |
Editor’s Note: As part of our “Year in Review” retrospective, we’ve selected the top 30 news stories of the year and are re-sharing them as we close out 2023. Follow along as we count down to number 1!
This story was originally published August 9, 2023.
No. 25 biggest news story of 2023:
The suggested workforce-to-population ratio required for adequate delivery of neuro-ophthalmology services has been estimated to be one specialist per 1.2 million people. However, in 2022 only eight US states met this threshold; in the worst-served areas, six had no neuro-ophthalmologists in the entire state. With increasing outpatient demand, and the subspecialty’s scarcity, one new study wanted to determine what the typical presentations to the emergency department (ED) for related issues look like.
The prospective study published by Ophthalmology included one academic care institution’s ED and inpatient neuro-ophthalmology consultation patterns and patient outcomes over one year. Of the 494 consecutive adult consultations, 49% took place at night or on weekends. Of the emergency consults (65%), 39% of these occurred during weekdays, 39% on weeknights and 22% on weekends/holidays. Of 322 ED consultations, 70% presented with a chief neuro-ophthalmic complaint.
Referrals to the ED by healthcare professionals were primarily made by eyecare specialists (76%, 196 patients). Most commonly encountered questions for emergency referral were due to papilledema at 23% and vision loss at 22%. A sizable 68% had a final active neuro-ophthalmic diagnosis, 69% had high or very high complexity and 44% needed admission.
Of the remaining 172 inpatient consultations, most were requested by hospitalists, including neurologists (41%) and oncologists (12%) for vision loss (25%) and eye movement disorders (20%), as well as neurosurgery (33%) to examine for mass or preoperative evaluation (11%). Active neuro-ophthalmic diagnosis was confirmed in 67% of patients, and a striking 90% of cases found neuro-ophthalmic assessment appropriate to make a diagnosis or evaluate for ophthalmic manifestations of disease. Follow-up with outpatient neuro-ophthalmology was required in 59% of patients.
The study authors note that overall, 61% of patients were diagnosed with a life- or vision-threatening pathology. Of the 49% of consultations occurring during off-hours, only 25% of these were urgent—highlighting “the paradoxical relationship between the additional burden generated by these unscheduled urgent neuro-ophthalmology consultations and the genuine need for these patients to be examined by a neuro-ophthalmologist, to whom limited access generates more such consultations.”
Driving the spikes in neuro-ophthalmology referrals or consultations are factors of delayed consultations resulting in diagnostic errors, increased cost and worse outcomes, made worse by associated risk for litigation for the provider if not done promptly. Further motivation for patient referral to hospitals than outpatient clinics is that ED or hospital evaluation is time efficient, which allows for immediate multidisciplinary care and testing which may be delayed otherwise with outpatient settings.
To deal with the rising rates, the authors propose that increasing the number of available outpatient neuro-ophthalmologists may be one solution. They also propose that “there is a need for expanded development and utilization of technological and diagnostic aids such as nonmydriatic fundus cameras in EDs as well as telehealth delivery processes for integration into healthcare settings. Finally, creating and implementing standardized neuro-ophthalmology ED and hospital protocols for commonly encountered presentations and diseases should facilitate rapid diagnosis and treatment of common neuro-ophthalmologic disorders.”
Smolar ALO, Ray HJ, Dattilo M, et al. Neuro-ophthalmology emergency department and inpatient consultations at a large academic referral center. Ophthalmology. August 4, 2023. [Epub ahead of print]. |

