 |
Several weeks ago, I received a call from an acquaintance who asked if I was interested in rendering a second opinion for a colleague of hers who was unsure of the management plan a glaucoma specialist had recently prescribed for her patient. Since this is clearly in my wheelhouse, I accepted and saw the patient earlier this year, in September. Here’s what I found.
Case
The patient was a 38-year-old Caucasian female who had been diagnosed with glaucoma earlier this year in both eyes, but it was her left eye that was of most concern. She had gotten the impression that she would soon lose significant vision if the situation was not brought under control as soon as possible.
 |
|
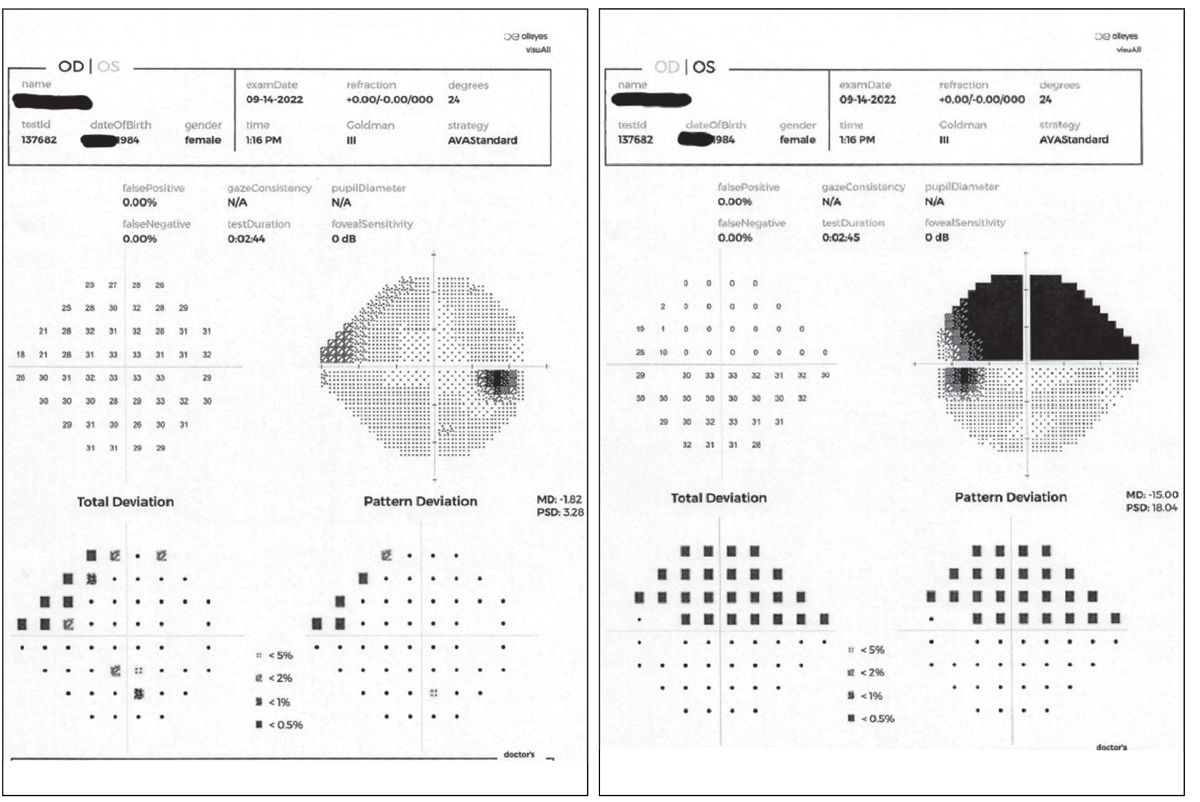
The patient’s right and left visual fields on presentation. Pre-dilation testing showed an early nasal step defect OD and a significant altitudinal defect involving fixation OS. Click image to enlarge. |
Her glaucoma medications included latanoprost HS OU, netarsudil QD OU and simbrinza BID OU. She reported that the netarsudil had been added most recently—a few months ago—and said she was told that she would be heading toward laser surgery in the left eye if it did not offer adequate control. Other than oral contraceptives, she was not taking any other medications. She reported good compliance with her drop regimen, and there was no evidence of medication intolerance. She had no allergies to medications but reported a family history of glaucoma in her father and maternal grandfather.
 |
|
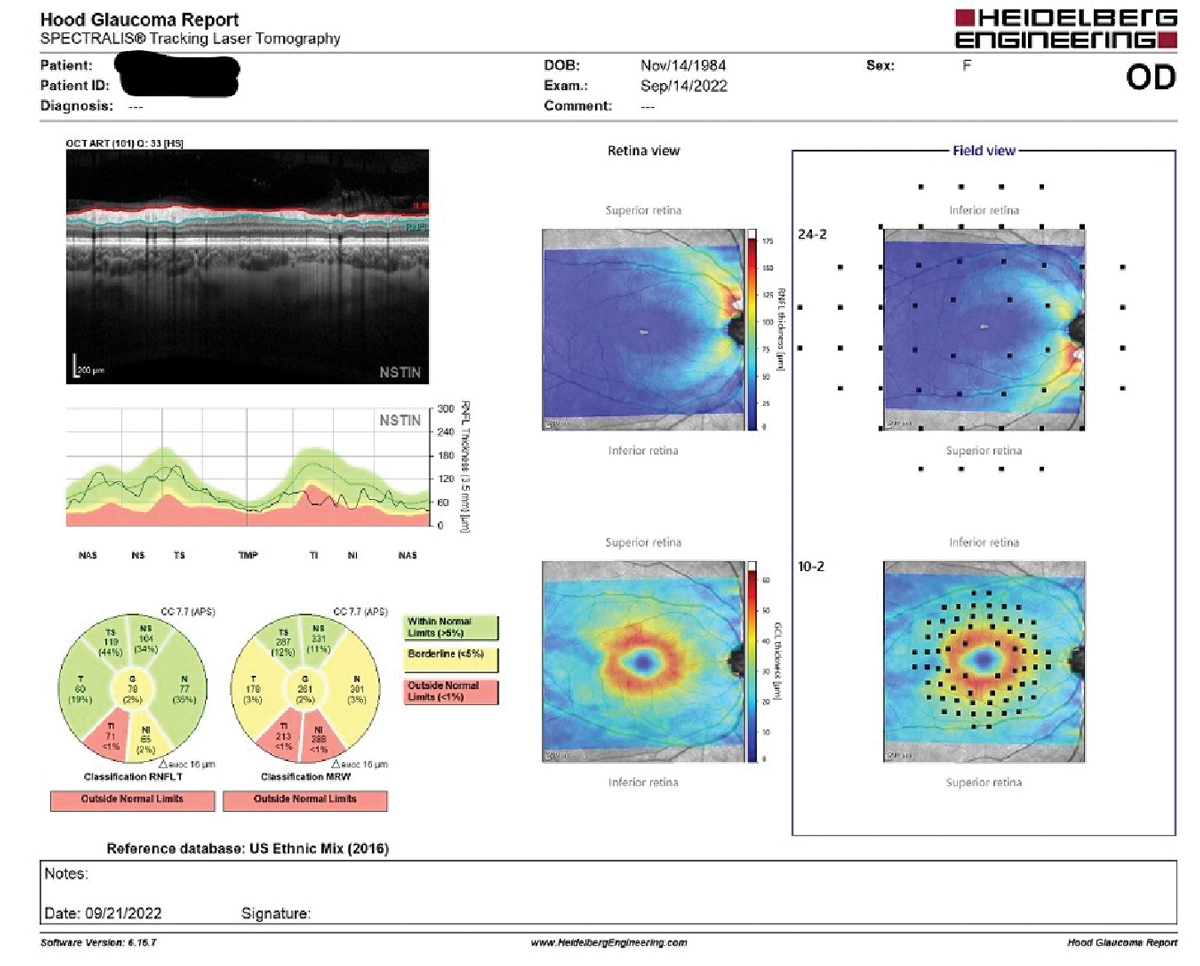
On the lower left of the Hood report, note the Garway-Heath sector aberrations in both the RNFL and MRW readings inferotemporally. The RNFL defects are also seen on the NSTIN graph in the middle left of the image. Additionally, there is a wedge defect in the RNFL map in the central column top image under the retina view. Note too the relatively normal ganglion cell map in the lower portion centrally of the image under the retina view. Click image to enlarge. |
Her entering visual acuities were 20/20 OD and 20/30- OS through minimally myopic spectacles. Pinhole acuities slightly improved to 20/30+ OS. Her pupils were ERRLA with no afferent defect, and her extraocular muscles were full in all positions of gaze.
A slit lamp exam of the anterior segment was unremarkable. The patient’s angles were wide open by Van Herick estimation. Her applanation pressures were 16mm Hg OD and 17mm Hg OS. Pachymetry readings were 552µm OD and 560µm OS.
Prior to dilation, threshold 24-2 visual field testing showed an early nasal step defect OD and a significant altitudinal defect involving fixation OS.
On dilated fundus examination, the patient’s crystalline lenses were clear. Her cup-to-disc ratio was 0.50x0.50 OD, with the left disc too difficult to assess because it was a significantly obliquely inserted disc. The neuroretinal rim in the right eye at the slit lamp was plush and well perfused; that of the left demonstrated a very thin inferior neuroretinal rim from three to nine o’clock, owing to the extremely vertically inserted anatomy. The retinal vasculature was normal OU, as were the maculae, though there was no foveal reflex OS. The peripheral retinal evaluation was normal.
Once dilated, OCT imaging of both optic nerves and maculae was obtained. In particular, I was interested in all three regions where glaucomatous damage may be evident: at the BMO-MRW indices (neuroretinal rim), the perioptic RNFL and the macula.
Imaging supported the in vivo slit lamp results. In the right eye specifically, there were some expected findings and a couple that raised concern for early glaucoma. Normal was the macular ganglion cell thickness. Abnormal was a small RNFL inferior arcuate defect that extended to the optic nerve, which also showed BMO-MRW thinning inferotemporally. These structural defects coincided with the early nasal step seen in the right field.
 |
|
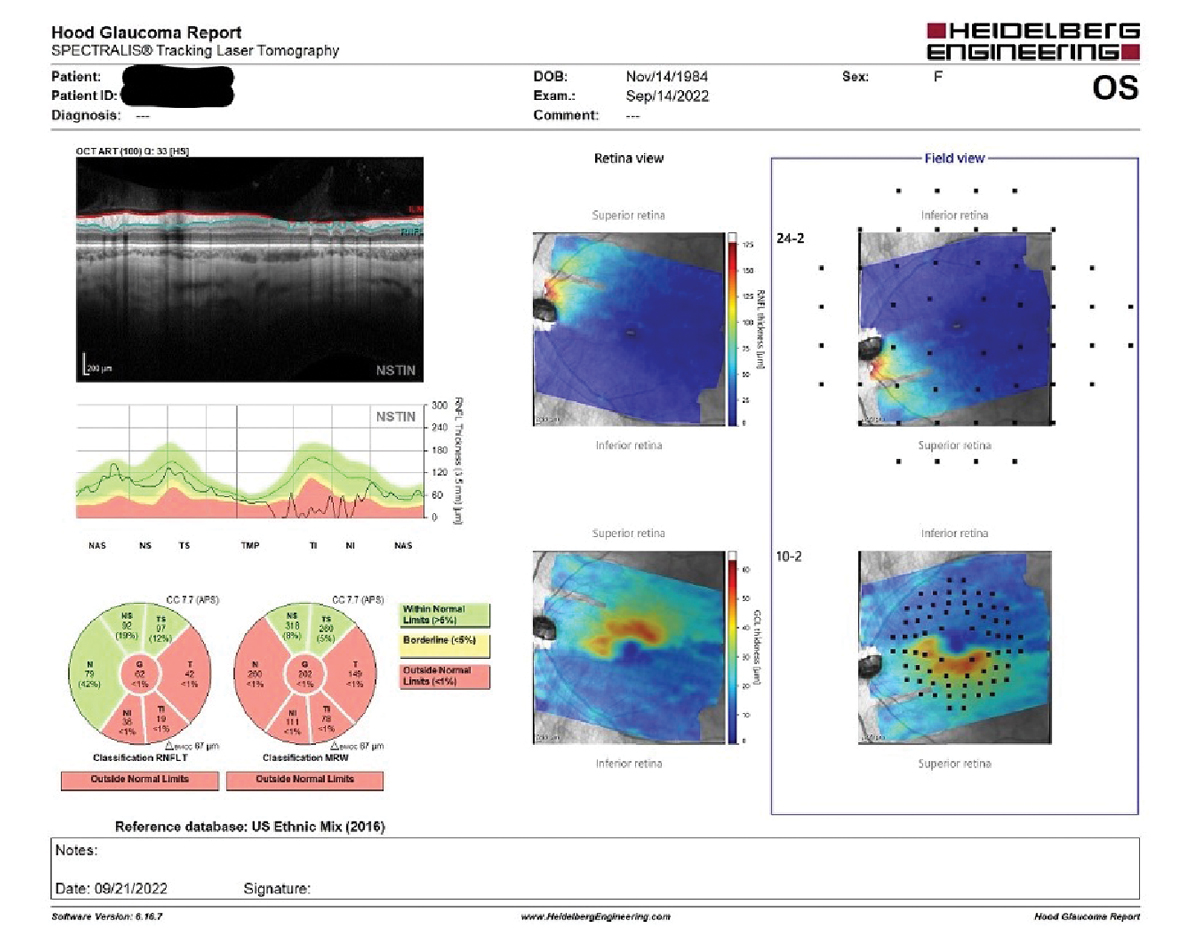
Note in the field view, to the far right in the image, the retinal thinning seen in the tilted disc on the left coincides nicely with the superimposed visual field test points, which in turn match perfectly with the results seen in the visual field study. Click image to enlarge. |
OCT of the left eye was notable for several reasons. The first was the paucity of retinal tissue seen in the retinal views of both the RNFL and the macular ganglion cell layers inferiorly. This is related to the obliquely inserted nerve and inferior hypoplastic tissue in the nerve and retina coinciding with the significant field defect in the left eye. Likewise, on the RNFL and MRW scans, there was significant absence of robust neuroretinal rim and RNFL tissue inferiorly in the right nerve. These findings are consistent with tilted disc syndrome. The loss of retinal tissue and consequently RNFL and neuroretinal rim tissue covers a large portion of the inferior anatomy of the retina and optic nerve and involves fixation.
Discussion
Tilted disc syndrome is congenital. Typically, the superior visual field is involved, and visual acuities may be affected depending on the severity of the angle of approach and insertion of the optic nerve to the sclera. Tilted disc syndrome is most commonly found in highly myopic eyes, and visual field progression often occurs in these patients.1 Our patient was a low myope of -1.50D spherical equivalence.
Interestingly, it has been suggested that patients with tilted disc syndrome may actually have a lower likelihood of progressive glaucomatous damage, which may not come as too much of a surprise due to the relationship between myopia and glaucoma.2
There are many situations that mimic glaucoma both structurally and functionally, and tilted disc syndrome is one of them. So the obvious question here is this: since there are significant structural and functional changes seen in the left eye, is this a case of mistaken identity? In other words, are we not looking at glaucoma but simply the effects of a tilted disc?
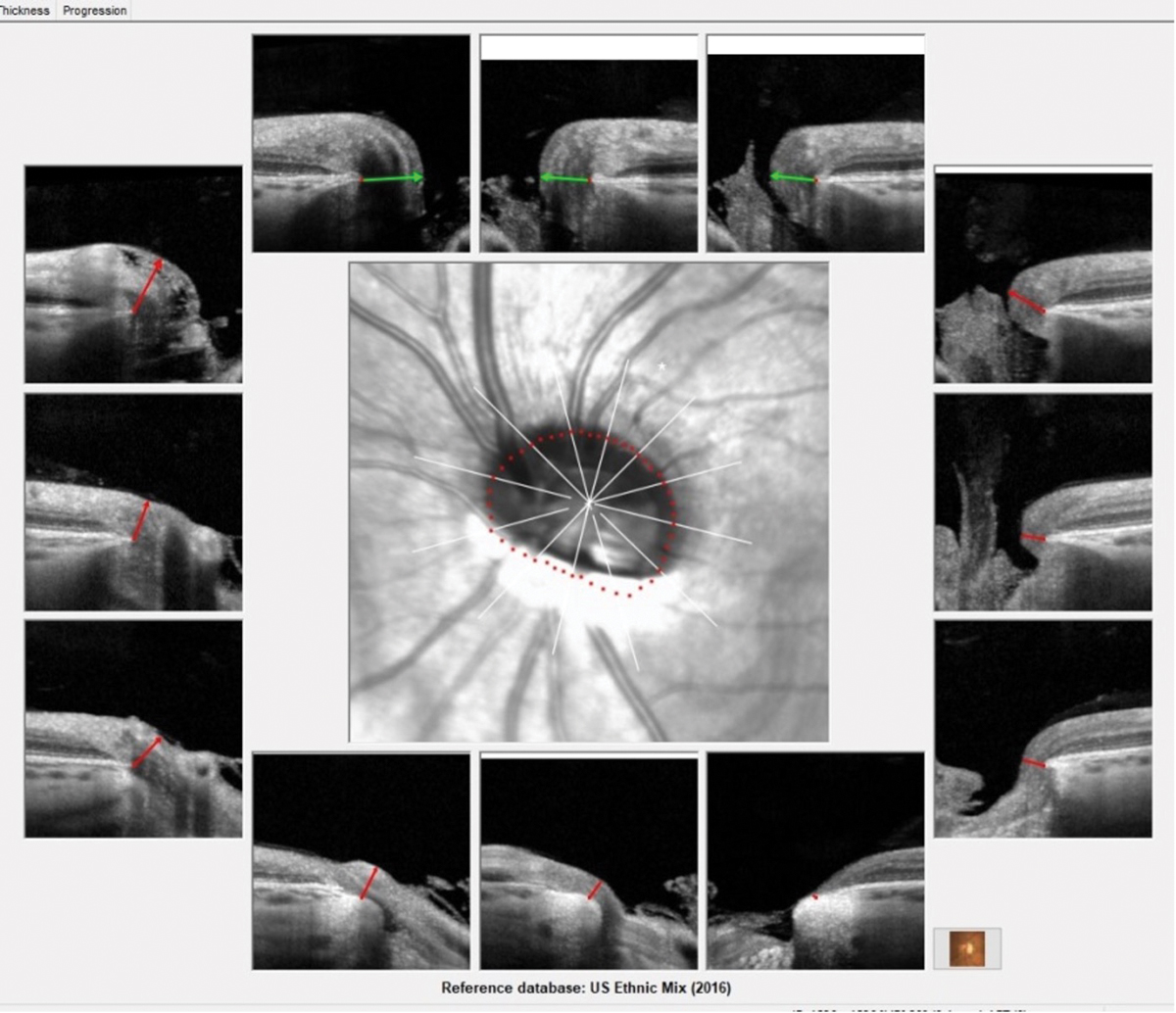 |
| Note the inferiorly inserted approach of the optic nerve OS, as well as peripapillary atrophy visible inferiorly. In particular, note especially the significantly thin, colobomatous lack of tissue of the neuroretinal rim seen in the five o’clock representative image. The severe angle of insertion of the left optic nerve can be appreciated on the BMO-MRW printout of the left eye. Click image to enlarge. |
Well, there is no doubt that the tilted disc in the left eye plays a role in interpreting the clinical findings; however, the right optic nerve has absolutely no clinical appearance of a tilted disc but does have clinical findings associated with early glaucoma. While I would concur that there is early evidence of glaucoma in the right eye, it is hard to determine how much damage in the left eye is attributable to glaucoma vs. the tilted disc.
However, from a practical perspective, since the tilted disc is rather significant, I would assume at this point that the significant structural change is associated with the tilted disc, with perhaps some damage due to glaucoma. Given the fact that the right eye shows glaucomatous damage in the early stage in a patient with a family history of glaucoma, I’d also assume the left will eventually follow on the same path.
While I do think the patient is currently overmedicated topically for glaucoma, I chose to not change any medications at this point, obtain her previous records to ascertain any notable changes that happened previously to warrant a ratcheting up of her medication regimen and reassess her OCTs in six weeks. If they are stable at the follow-up, we’ll begin a slow reduction in her medication regimen to a level where we can keep her on the fewest number of drugs while at the same time making sure the glaucoma does not progress to more severe stages.
Dr. Fanelli is in private practice in North Carolina and is the founder and director of the Cape Fear Eye Institute in Wilmington, NC. He is chairman of the EyeSki Optometric Conference and the CE in Italy/Europe Conference. He is an adjunct faculty member of PCO, Western U and UAB School of Optometry. He is on advisory boards for Heidelberg Engineering and Glaukos.
1. Tanaka Y, Shimada N, Ohno-Matsui K. Extreme thinning or loss of inner neural retina along the staphyloma edge in eyes with pathologic myopia. Am J Ophthalmol. 2015;159(4):677-82. 2. Lee JE, Sung KR, Lee JY, Park JM. Implications of optic disc tilt in the progression of primary open-angle glacoma. Invest Ophthalmol Vis Sci. 2015;56(11):6925-31. |

