 |
|
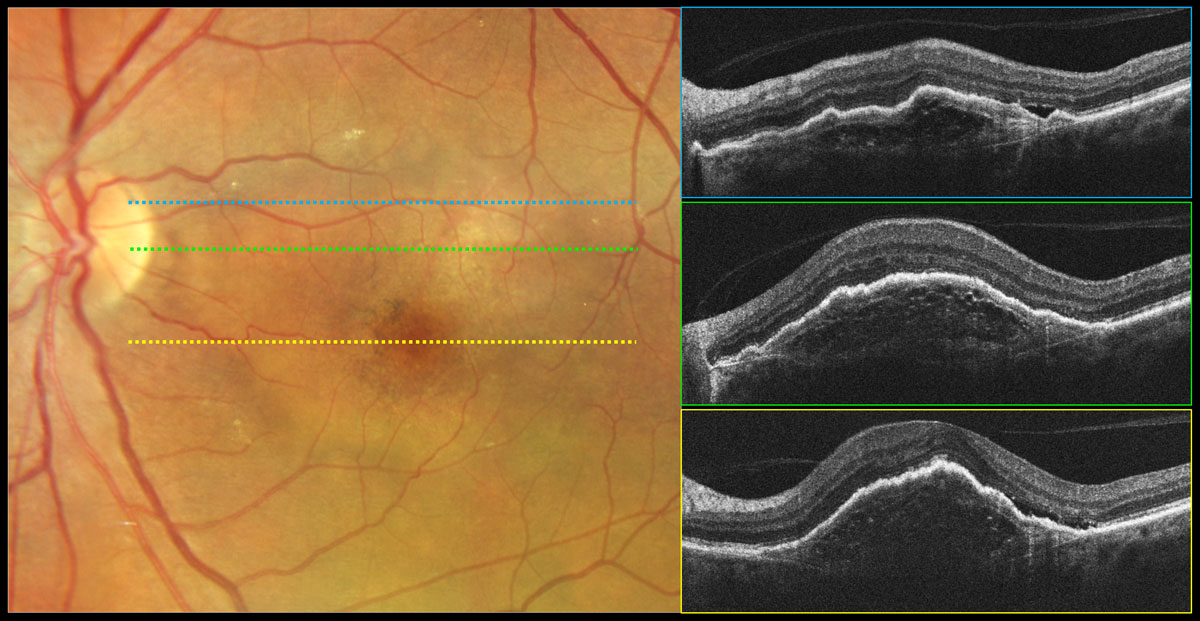
Beware of fibrotic scar when imaging nAMD patients, as fibrosis is known as one of the condition’s end-stage—and vision-threatening—sequelae. Photo: Carolyn Majcher, OD. Click image to enlarge. |
Around 40% of patients with neovascular age-related macular degeneration (nAMD) have fibrosis at two years of treatment, and at 10 years, the incidence is as high as 70%. Fibrosis has been associated with poorer visual outcomes in patients with nAMD. It can be challenging to identify a fibrotic scar in a patient with nAMD, and there’s also a lack of imaging guidelines for its diagnosis. In a new study published in the American Journal of Ophthalmology, researchers performed a systematic review and meta-analysis to report on the diagnosis, epidemiology, risk factors and visual outcomes of fibrosis to help shed more light on the condition.
Thirty-seven relevant articles were selected from PubMed including the following search terms: age-related macular degeneration or age-related maculopathy and fibrosis, scar, scarring, fibrovascular or fibrotic. There were 29 real-world studies and eight randomized controlled trials reviewed, most of which used multimodal imaging such as color fundus photography, fluorescein angiography, fundus autofluorescence, OCT, OCT-A and/or polarization-sensitive OCT.
Across all the studies reviewed, the prevalence of fibrosis in nAMD patients at baseline, 12, 24 and 60 months was 13%, 32%, 36% and 56%, respectively. The researchers pointed out that fibrosis development seemed to be highest in the first year and slow down over time. In their paper on the study, they wrote, “Approximately 60% of the fibrosis burden in nAMD at five years is present in the first year of treatment.”
The following risk factors for fibrosis were observed: classic choroidal neovascularization (CNV), intraretinal fluid, hemorrhage, hyperreflective material, CNV lesion size and retinal thickness. On the other hand, subretinal fluid and pigment epithelial detachment appeared to be protective factors. The two treatment-associated factors were disease activity and time to diagnosis.
Importantly, the data highlighted the magnitude of visual impairment associated with the condition; patients with fibrosis had worse best-corrected visual acuity at baseline than those without the condition by -18.5 letters. After one year with or without treatment, this value decreased to -26.86 letters.
Because this study and previous ones have shown that fibrosis worsens more in the first year than in the years following in patients with nAMD, developing standardized recommendations for diagnosis using the various imaging modalities is crucial to aid in sooner detection and earlier intervention.
“There is a need to identify effective treatment strategies for fibrosis and to monitor at-risk patients closely. More studies involving multimodal imaging are required to clarify the definitions and grading criteria for fibrosis,” the researchers concluded.
Cheong KX, Cheung CMG, Teo KYC. Review of fibrosis in neovascular age-related macular degeneration. Am J Ophthalmol. September 23, 2022. [Epub ahead of print]. |

