Identifying the association between chronic kidney disease (CKD) and the progression of ocular neuronal damage is important to improve patient screening, but the relationship between CKD and ganglion cell-inner plexiform layer (GCIPL) thickness isn’t clear. In a new study, researchers assessed the cross-sectional and longitudinal associations between the two and found that those with poorer renal function exhibited thinner GCIPL, and GCIPL thickness declined more rapidly.
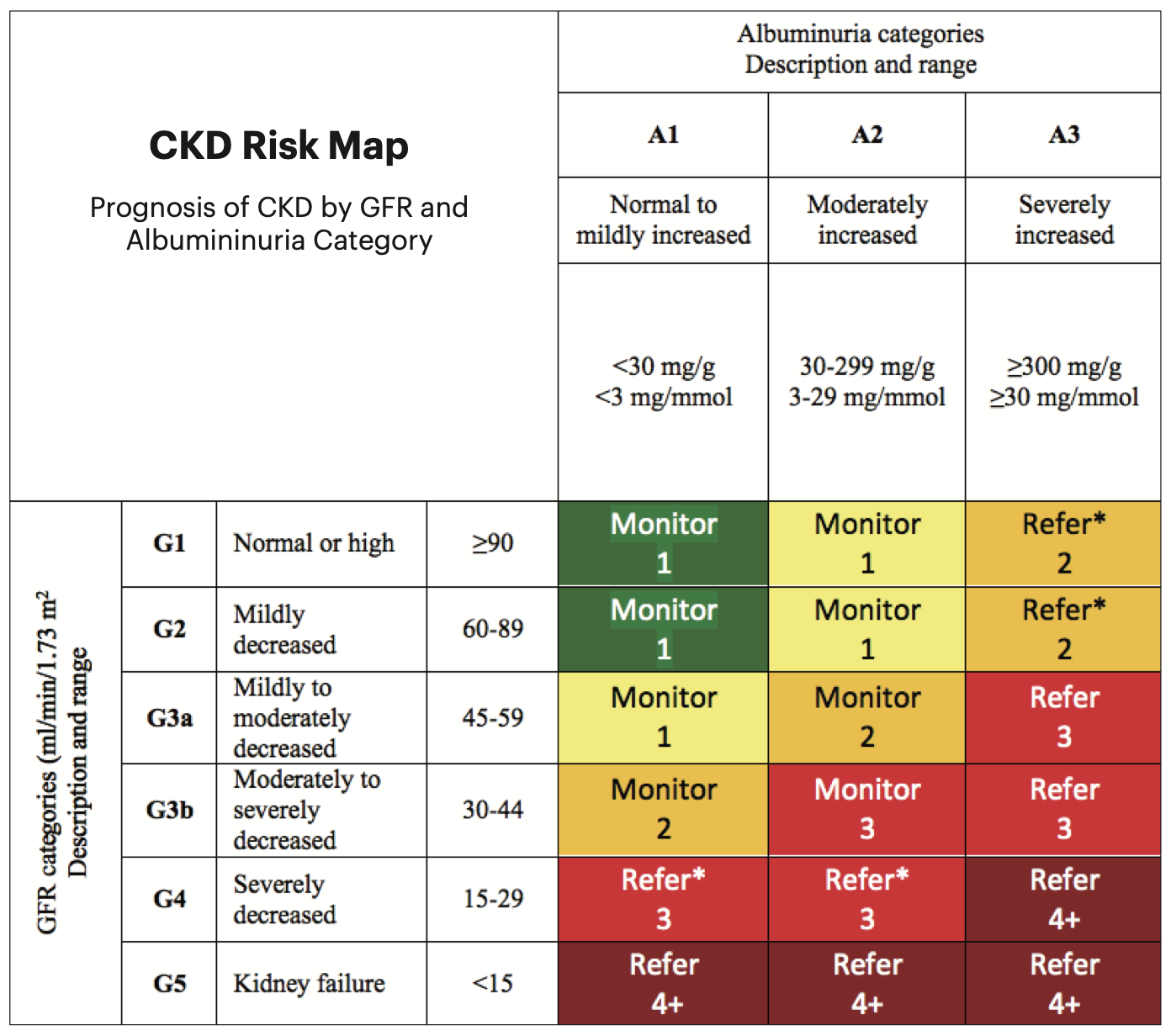 |
| Renal function influences the rate of GCIPL decline in those with diabetes and hypertension, suggesting that renal impairment is a risk factor for neuronal damage. Photo: National Kidney Foundation. Click image to enlarge. |
This study included 23,014 without neurodegenerative diseases individuals from the UK Biobank and three years of annual follow-up data of 2,197 individuals from a Chinese cohort. Three groups were defined by estimated glomerular filtration rate based on serum creatinine. CKD severity was classified as no CKD, mild-CKD or moderate-to-severe CKD (MS-CKD). The GCIPL thickness by OCT was analyzed over time to determine its decline rate in micrometers per year. Linear regression models were used to assess the correlation between renal function and both the baseline GCIPL thickness and the GCIPL decline rate.
The cross-sectional analysis (in a largely white population) showed that poorer renal function negatively correlated with GCIPL thickness (0.15μm thinner in mild-CKD and 0.83μm thinner in MS-CKD, on average). Longitudinal analysis in the Chinese cohort showed that the GCIPL decreased more rapidly in individuals with poorer renal function. “After correcting for all confounding factors, the rate of GCIPL thinning was 0.30μm/year more in the mild-CKD group and 0.52μm/year more in the MS-CKD group, compared to controls without CKD,” the authors explained in their paper for American Journal of Ophthalmology. This was sustained in those with diabetes or hypertension, they noted.
“Importantly, these associations were independent of other known risk factors, suggesting that renal function impairment may contribute to neuronal damage and that controlling renal function may help prevent the onset of neurodegenerative diseases,” the authors wrote.
These results have important implications for public health and clinical practice, the authors suggested. “Firstly, they support the concept that ‘the eye is a window to the whole body,’ as the neurosensory retina allows noninvasive in vivo visualization of the microvascular circulation and central nervous system, making it an ideal environment for characterizing systemic diseases such as cardiovascular disease, aging and dementia.” The study found a negative correlation between CKD severity and GCIPL thickness.
“Secondly,” they continued, “as OCT imaging becomes more widespread in primary care and ophthalmology settings, it can be used to measure the risk of neuronal injury progression by including renal function as an additional screening measure.”
Third, the researchers noted, renal function should be considered when interpreting future clinical reports to avoid incorrect diagnoses.
“Lastly, previous studies on factors related to GCIPL have reported contradictory results, possibly because they did not consider renal function as a confounding factor,” the authors concluded.
These results suggest that renal impairment is a risk factor for neuronal damage, and future studies are needed to investigate whether preserving renal function can slow down neurodegenerative diseases progression, the authors summed up.
Guo X, Zhu Z, Bulloch G, et al. Cross-sectional and longitudinal association of chronic kidney disease on retinal neurodegeneration: a cross-cohort analysis. Amer J Ophthalmol. October 3, 2023. [Epub ahead of print.] |

