 |
|
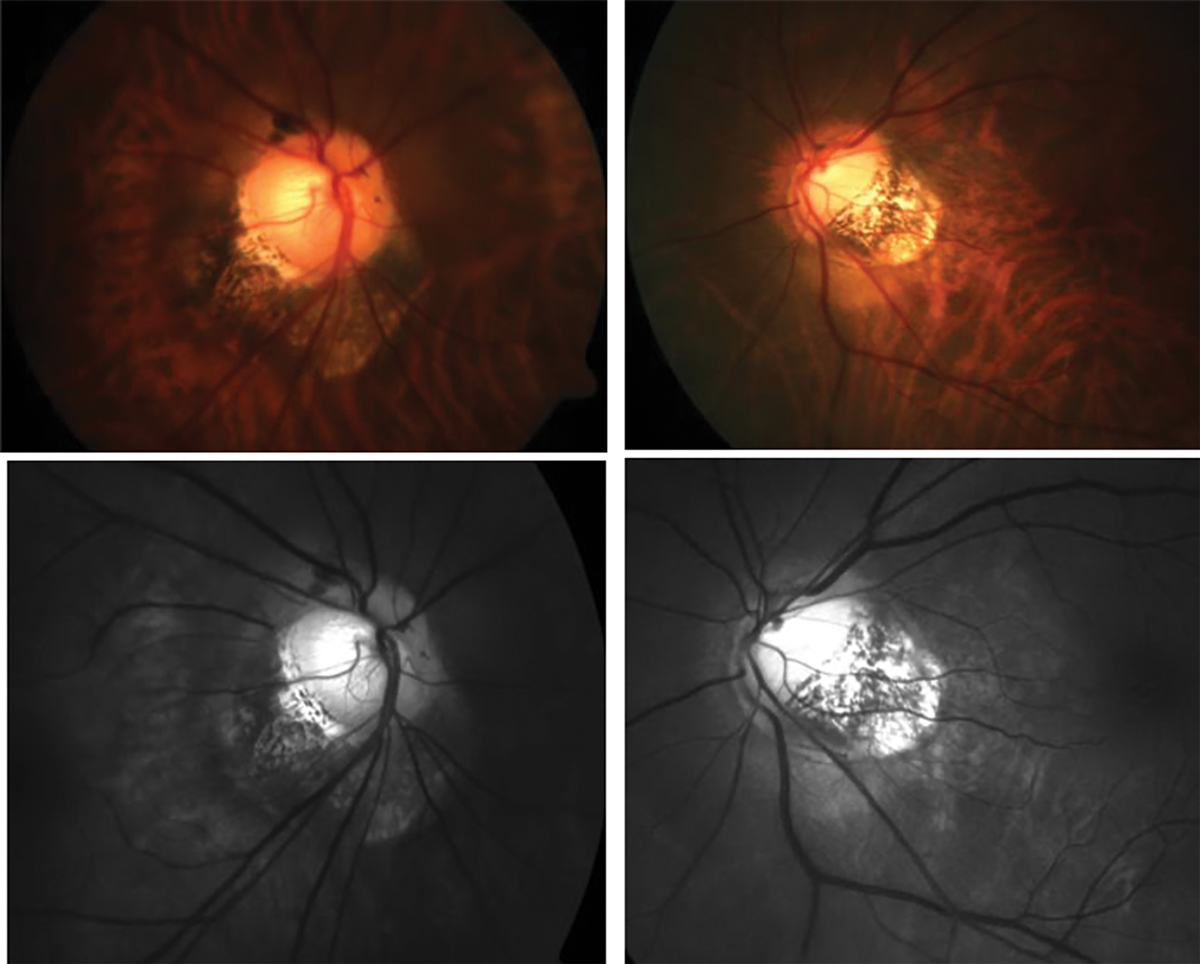
Anomalous optic nerve insertion, tilting and torsion and posterior staphyloma in a highly myopic patient. Photo: Andrew Rouse, Lauren Sabol, Tej Ramdass. Click image to enlarge. |
It’s not a novel concept that some association seems to exist between the two conditions, but this research, as seen in Ophthalmology, wanted to take a different approach to come closer to an explanation. Most studies that outline a connection between myopia and primary open angle glaucoma (POAG) are observational and specify that myopic eyes are at greater risk of POAG development, but with inconsistent evidence. Potential confounding factors leading to this problem arise from myopia, making clinical tests for glaucoma more complicated.
Looking to combat this issue, researchers used Mendelian randomization analysis to overcome the confounding influences of external variables. From this analysis, researchers were able to make a genetic causal association between myopia, glaucoma and glaucoma-related traits.
Data were collected from the largest publicly available genetic banks, which ranged in sample size from 216,257 to 542,934 individuals. Multiple models were constructed to identify any significant mediators between the two conditions.
What was found was a consistent bidirectional genetic association between the two conditions, as well as intraocular pressure (IOP). IOP displayed a bidirectional genetic association with myopia as well. Genomic modeling revealed that IOP was a confirmed mediator in causal association between myopia and POAG. Interestingly, myopia also showed a causal effect on optic disc area, yet an effect of optic disc area on myopia was not uncovered.
The researchers highlight some of the mechanisms that have been proposed in the underlying reason for association between myopia and POAG. One possibility is elongation of the lamina cribrosa and thinning caused by axial elongation and optic disc enlargement. As a result, a lesser distance between the intraocular and retrobulbar compartments of the eye could result in a steeper translaminar pressure gradient. This increased pressure is believed to predispose glaucomatous injury to retinal ganglion cell axons.
Even further, axial elongation as a result of myopia is proposed to also underlie glaucoma pathogenesis. Through the elongation process, biomechanical and ischemic processes that cause retinal thinning of RGC layers could be at work.
As for the involvement with IOP and myopia, structural changes of the optic nerve head exhibited in glaucoma may be the result of raised IOP. In turn this may contribute to posterior pole lengthening, and thus a myopic shift change.
The authors contend that the genetic causal link between the conditions could mean that treatments for stopping myopia progression also could modulate glaucoma risk. Myopia’s link to glaucoma is evidently mediated by IOP, thus “this may imply possible therapeutic benefits of IOP-lowering treatment on alleviating retinal ganglion cell injury associated with progressive myopic optic neuropathy—even in the absence of a clear clinical diagnosis of glaucoma, which is often challenging to establish in myopic eyes,” they wrote in their paper.
Chong RS, Li H, Cheong A, et al. Mendelian randomization implicates bidirectional association between myopia and primary open angle glaucoma or intraocular pressure. Ophthalmology. 2022. [Epub ahead of print]. |

