 |
Q:
I have several patients who don’t respond to medical and mechanical dry eye therapies such as prescription drops, LipiFlow (Johnson + Johnson) or BlephEx. What are my next steps?
Dry eye disease (DED) has been identified as a multifactorial condition, and there are myriad treatment options to address its causes. But when those fail, we must ask, “Are we missing a bigger picture?” Recent studies have shown that modern lifestyles can contribute to DED, whether it is digital screen use, increased stress or poor sleep and nutrition.1
“I believe including lifestyle modifications in our dry eye management should be the standard of care in treating DED,” says Mila Ioussifova, OD, of South Waterfront Eyecare in Portland, OR.
 |
|
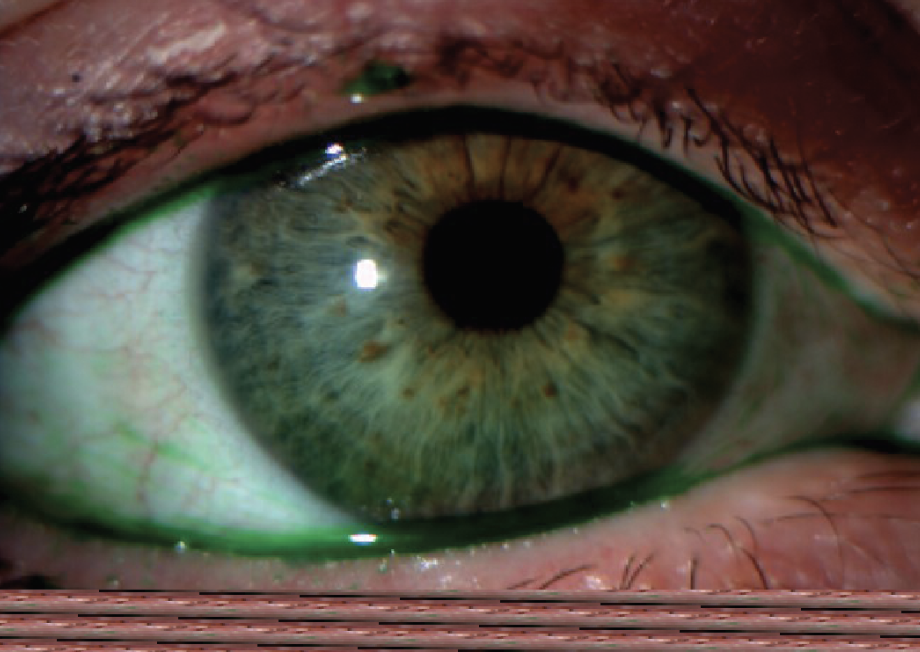
Fig. 1. Ocular rosacea and meibomian gland dysfunction. Click image to enlarge. |
Underlying Trouble
With more advanced dry eye treatments like intense pulsed light (IPL), we have learned about the correlation between rosacea and DED, according to Dr. Ioussifova. Rosacea is a common dermatological condition that often manifests with ocular complications like meibomian gland dysfunction (Figure 1) and Demodex blepharitis.2,6
Rosacea is also a complex and multifactorial disease, one in which imbalances in the skin organisms have been identified as its pathogenesis.3 Recent studies have described that these alterations are due to gut dysbiosis, the alterations in the gastrointestinal (GI) microbiome and its associated pathologies, such as small intestinal bacterial overgrowth, irritable bowel syndrome and inflammatory bowel disease.5 Consider these issues when treating rosacea and dry eye with IPL yet still noting recurrent flare-ups.
Many pharmaceutical treatments aid to reduce inflammation involved with DED. However, oxidative stress and the dysregulation of redox homeostasis could potentially play a causative role in the inflammatory process and pathogenesis of dry eye.
Studies have shown that patients with DED exhibit higher levels of oxidative stress markers in tears and conjunctival cells and lower levels of antioxidant enzymes, leading to peroxidation of lipids on the ocular surface and DNA oxidative damage in both nuclei and mitochondria, resulting in loss of goblet cell density in the conjunctiva.4
Healthy Body, Healthy Eyes
“When managing dry eye patients, we are given an opportunity to look at and treat the whole person by assessing the imbalances in their body to maximize nutrient absorption, antioxidant support and improve detoxification pathways—especially important in those with autoimmune conditions,” Dr. Ioussifova emphasizes. “Incorporating nutrition and lifestyle modifications has been crucial in managing some of my most challenging dry eye patients.”
She recommends ordering functional testing to assess micronutrient or hormonal imbalances, as well as assessing GI microbiome dysbiosis with stool testing. Ask patients how many hours they sleep, how many times a week they exercise, what they usually eat and how they feel after meals to sense if they have GI disturbances. “You would be surprised how many people report they have GI issues but think those symptoms are normal,” she observes. “We may be their first provider to make the connection between their gut symptoms and their rosacea and dry eye flare-ups.”
Dr. Ioussifova’s favorite comment from her patients is, “I came to you for my eyes, but now my skin is better, my stomach is happier and I have better sleep and more energy.”
“When we treat the imbalances in the gut, the root cause of most non-communicable diseases and address other lifestyle factors, we can help heal the patient’s whole body, not just the eyes,” she says.
Dr. Ajamian is board certified by the American Board of Optometry and serves as Center Director of Omni Eye Services of Atlanta. He is vice president of the Georgia State Board of Optometry and general CE chairman of SECO International. He has no financial interests to disclose.
1. Markoulli M, Arcot J, Ahmad S, et al. TFOS lifestyle: impact of nutrition on the ocular surface. Ocul Surf. April 25, 2023. [Epub ahead of print]. 2. Andreas M, Fabczak-Kubicka A, Schwartz RA. Ocular rosacea: an under-recognized entity. Ital J Dermatol Venerol. 2023;158(2):110-6. 3. Daou H, Paradiso M, Hennessy K, Seminario-Vidal L. Rosacea and the microbiome: a systematic review. Dermatol Ther (Heidelb). 2021;11(1):1-12. 4. Navel V, Sapin V, Henrioux F, et al. Oxidative and antioxidative stress markers in dry eye disease: a systematic review and meta-analysis. Acta Ophthalmol. 2022;100(1), 45-57. 5. Wang FY, Chi CC. Rosacea, germs, and bowels: a review on gastrointestinal comorbidities and gut-skin axis of rosacea. Adv Ther. 2021;38(3):1415-24. 6. Gonzalez-Hinojosa D, Jaime-Villalonga A, Aguilar-Montes G, Lammoglia-Ordiales L. Demodex and rosacea: Is there a relationship? Indian J Ophthalmol. 2018;66(1):36-8. |

