 |
|
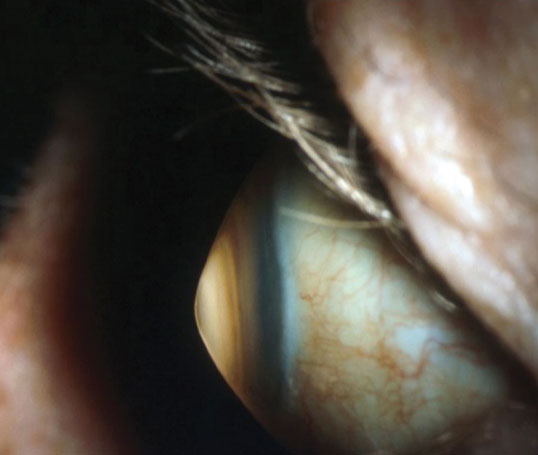
Keratoconus patients in this study scored lower on both visual function and socio-emotional QoL scales compared with controls. Click image to enlarge. |
One new study appearing in Cornea looked to identify both optical and visual components of vision-related quality of life (VR-QoL) in keratoconus patients. For patients with this condition, factors related to quality of life have been less explored, hence the further research.
The study was a cross-sectional, case-controlled, prospective design and included patients who were previously diagnosed with keratoconus as well as volunteers with healthy, emmetropic or ametropic eyes. A total of 77 patients with keratoconus were included and were age- and sex-matched for one-to-one controls.
To determine vision-related quality of life, assessments were done for autorefraction, high-contrast visual acuity testing, corneal imaging, intraocular straylight analysis, contrast sensitivity, aberrometry and performance on the National Eye Institute Visual Functioning Questionnaire. The Rasch-modified visual functioning scale and socio-emotional scale were used to quantify VR-QoL.
Researchers found that both the visual function and socio-emotional scores were significantly lower in keratoconus patients when compared to controls. Additionally, keratoconus patients exhibited poorer higher- and lower-order aberrations, high-contrast visual acuity and contrast sensitivity.
Strong predictors of socio-emotional score included spectacle-corrected high-contrast visual acuity, a higher spatial frequency contrast sensitivity and higher-order aberration metrics. Higher-order aberration (HOA) of the worse eye was also a strong predictor of socio-emotional and visual function score.
The researchers point out that these findings are consistent with what is already known about keratoconus, as a significant increase in HOA has been previously documented, especially for coma. The hypothesis correlating with this fact is that these optical errors might be what’s mainly causing visual impairment seen in keratoconus. The observed strongest predictor of HOA for social-emotional and visual function scores subscales of all measures corroborates this hypothesis.
Researchers additionally found forward light scatter, or straylight, correlations with keratoconus to be low. Consistent with previous research, this might indicate only a small effect of keratoconus on light scatter when significant stromal scarring or corneal surgery, like crosslinking, are absent. This might be the case especially when comparing these to induced optical aberrations, which consist of a much larger amount.
Despite straylight’s relatively smaller impact on visual quality compared to HOA, the model researchers used does display that straylight contributes an added value to HOA. As a result, this would explain some of the variance seen in VR-QoL for keratoconus patients.
The authors highlight their findings for use in real-world application. “Both higher and lower aberration showed a strong correlation with VR-QoL, surpassing high-contrast visual acuity. These findings underlie the importance of visual quality measures within keratoconus research and clinical care,” they explain, making this an important step when considering what to address when dealing with patients with this condition.
Schummer L, Kreps E, Pesudovs K, et al. Investigating the link between visual quality and vision-related quality of life in patients with keratoconus. Cornea. 2022. [Epub ahead of print]. |

