 |
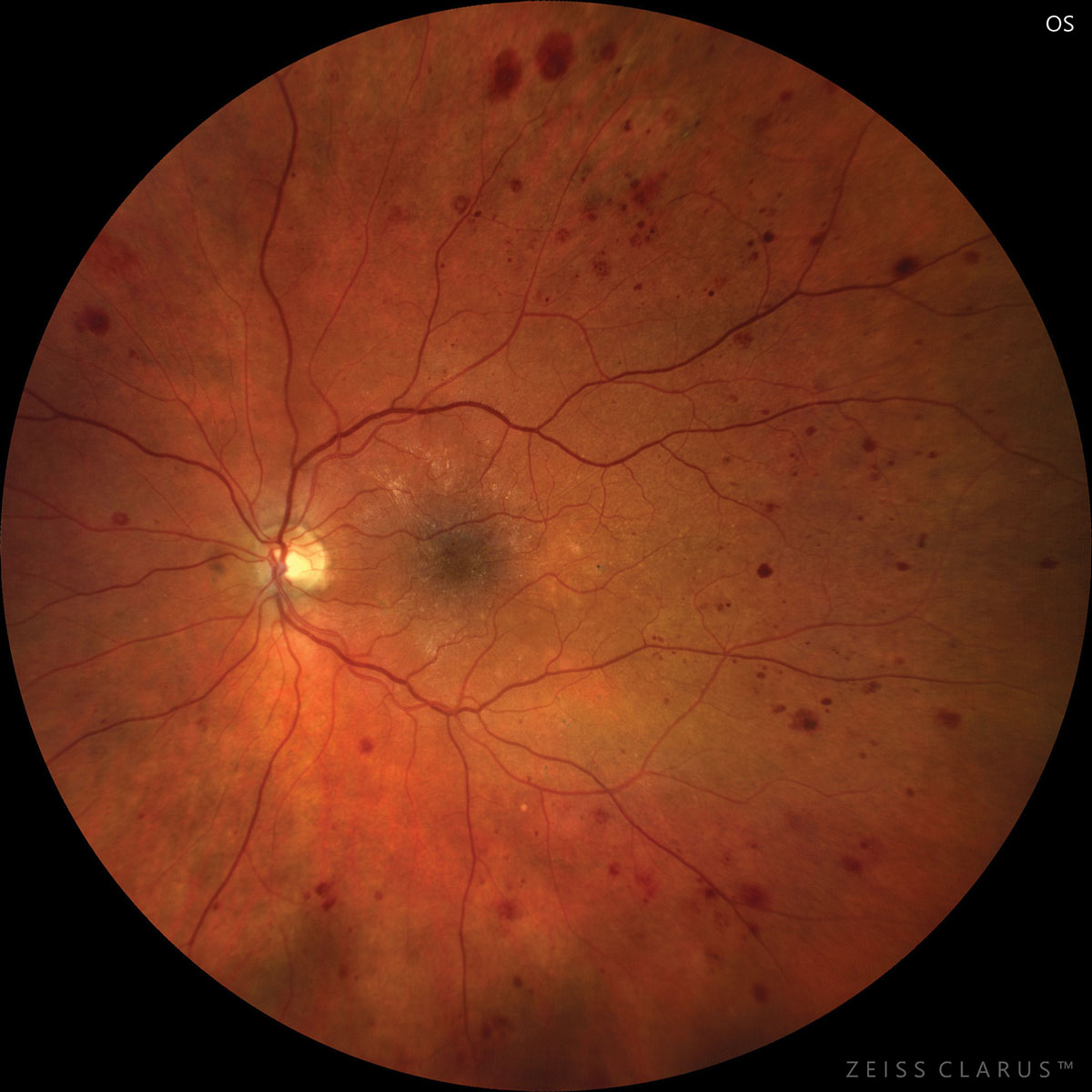
| Retinal neurodegeneration was to some extent affected by obesity and related metabolic disturbances. Photo: Jay Haynie, OD. Click image to enlarge. |
Although diabetic retinopathy (DR) is generally considered a microvascular complication, some evidence from both human and experimental animal studies have shown that neuroretinal deficits may occur in a very early stage, even before clinically detected microvascular lesions. Recent advancements in OCT make it possible to measure retinal individual layer thickness with its automated segmentation function. Researchers in China quantitatively evaluated the retinal neurodegenerative changes with retinal thickness parameters measured by macular OCT and found that neural damage occurred prior to the onset of clinical microvascular lesions in early diabetes.
The study included 102 type 2 diabetes patients without DR and 48 healthy controls in this observational, cross-sectional study. The OCT parameters of macular retinal thickness and ganglion cell-inner plexiform layer (GCIPL) thicknesses were evaluated between diabetic and normal eyes.
Macular retinal thickness and GCIPL thicknesses showed significant thinning in patients with type 2 diabetes. The most severe thinning was in the inferotemporal sector, and it was mildest in the superonasal and superior sectors. High BMI correlated with decreased GCIPL thickness and elevated intraocular pressure. A negative correlation between waist-to-hip circumference ratio and GCIPL thickness was also found. High-density lipoprotein and fasting C-peptide were associated with GCIPL thickness but only in the inferotemporal region. Multiple regression analysis showed that increased homeostasis model assessment scores independently predicted both average (β=-0.30) and inferotemporal (β=-0.34) GCIPL thinning. The study did not find a direct correlation between systemic factors and incident glaucoma; however, the researchers noted that obese type 2 diabetic patients with high insulin resistance scores have an increased risk of developing glaucoma.
“In the present study, the GCIPL of the type 2 diabetes mellitus patients without DR was 4% thinner than that of the healthy individuals. The percentage was larger than that in the overall retinal thickness (minus the GCIPL thickness), where the diabetes group was 1% thinner than controls,” they wrote in their paper. “It implies that relative to total retinal thickness, the GCIPL is affected to a greater degree in early diabetes.”
“The data from our study support that beyond ritual hypoglycemic measures, losing weight and improving insulin resistance and abnormal lipid metabolism are crucial to the management of early type 2 diabetic patients,” the team concluded in their paper.
Zheng Z, Yan M, Zhang D, et al. Quantitatively evaluating the relationships between insulin resistance and retinal neurodegeneration with optical coherence tomography in early type 2 diabetes mellitus. Ophthalmic Res. June 2, 2023. [Epub ahead of print]. |

