 |
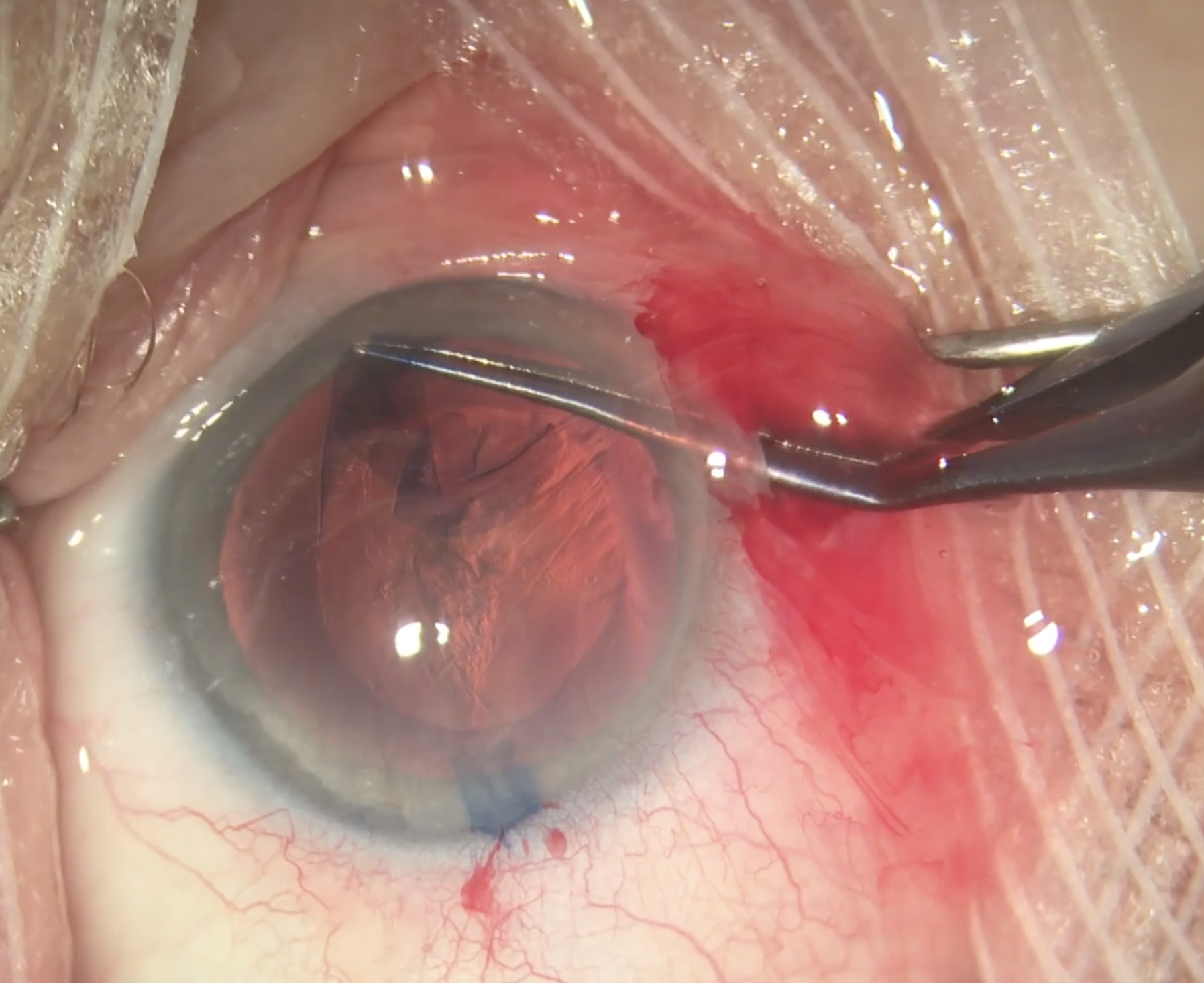
To ensure an uneventful cataract surgery, as seen here, be sure to carefully assess risk factors for PCR beforehand. A new study links intravitreal injection to risk elevation. Photo: Christina Tran, BS, and Leonid Skorin, Jr., DO, OD. Click image to enlarge. |
Cataract surgery and intravitreal injections are both very common and, by and large, very safe. But how does one influence the outcomes of the other? Posterior capsule rupture (PCR) during cataract surgery usually results in a longer and more complex procedure involving an anterior vitrectomy and a different IOL strategy. As identifying risk factors for PCR is key for planning cataract surgery, researchers recently performed a systematic literature review to assess the impact of previous intravitreal injection on the risk of PCR.
The researchers evaluated six studies (n=1,051,097 eyes) after conducting a literature search of 13 databases for studies that evaluated the risk of PCR in eyes undergoing cataract surgery that had had previous intravitreal injections. A total of 7,034 eyes had a history of previous intravitreal injection (the majority were anti-VEGF: 84% to 90% in three studies, 100% in three studies). The meta-analysis showed that any previous intravitreal injection was a risk for PCR (OR: 2.30).
“Compared with other known risk factors for PCR, previous intravitreal injection seems to be a risk factor of greater importance than axial length >26mm (OR: 1.47), small pupil size (OR: 1.45) or patient taking doxazosin (OR: 1.51); however, it seems to be a less important risk factor than surgeon training year one through two (OR: 2.83), pseudoexfoliation or phacodonesis (OR: 2.92),” the researchers wrote in their paper.
“However, when considering these numbers, it’s also important to realize that the risk from previous intravitreal injections is highly dependent on the number of previously performed injections,” they continued. “For each previous intravitreal injection, our meta-analysis found an OR of 1.04 for PCR. This OR can be converted to a relative risk factor for easier interpretation, which allows a more practical interpretation: a 4% increase in the risk of PCR for each number of previous intravitreal injections.”
The researchers say there are a number of potential mechanisms behind increased PCR risk after intravitreal injections. They listed four possibilities: “(i) iatrogenic physical trauma caused by the injection needle, (ii) changes in the mechanical properties of the lens capsule resulting from exposure to anti-VEGF or corticosteroids, (iii) accelerated cataractogenesis related to either anti-VEGF exposure or corticosteroids resulting in denser cataracts and (iv) denser cataracts because cataractous patients, who have concurrent retinal diseases that require intravitreal injection treatment, may have limited visual potential and are therefore perhaps referred for cataract surgery later compared with others. For the latter, however, it can also be argued that surgeons proceed to cataract surgery faster in subjects in an intravitreal injection treatment regimen due to the earlier diagnosis of cataract, as patients are continuously monitored.”
The researchers concluded that previous intravitreal injection raises the risk of PCR in cataract surgery and should be taken into consideration when planning cataract surgery. They noted, however, that a “substantial number” of previous injections (e.g., ≥10) are needed to qualify as a clinically significant PCR risk. This is because the a priori risk of PCR is very low (~1%), they wrote.
Bjerager J, van Dijk EHC, Holm LM, et al. Previous intravitreal injection as a risk factor of posterior capsule rupture in cataract surgery: a systematic review and meta-analysis. Acta Ophthalmologica. January 21, 2022. [Epub ahead of print]. |

