 |
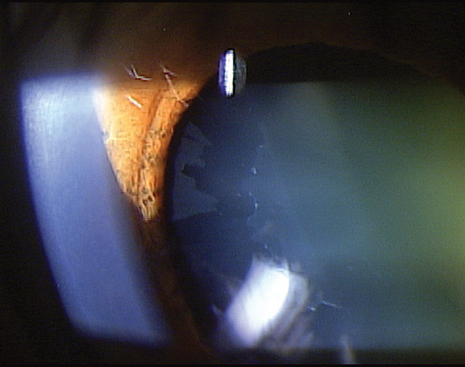
| The etiology of XFS may involve age-related processes that reflect the interaction of genetic and environmental factors, this study suggests. Photo: Michael Cymbor, OD. Click image to enlarge. |
Previous studies have shown that diabetes may be a risk factor for the development and progression of exfoliation syndrome (XFS), but the relationship between the conditions remains unclear. In a new literature review, researchers sought to clarify the association as a way to aid clinical strategies and shed light on disease pathogenesis.
Researchers evaluated 14 studies (nine cross-sectional and five case-control) comprising of 47,853 participants.
An inverse association was observed in studies that included older populations over the age of 65. The authors suggested that the etiology of XFS may involve age-related processes that reflect the interaction of genetic and environmental factors.
The results support the team’s hypothesis that a lower frequency of XFS may have been observed in older individuals with diabetes due to their long-standing hyperglycemic state, which can result in greater levels of advanced glycation end-products (AGEs), they proposed in their paper on the work for Ophthalmology Science.
Greater AGEs may result in abnormal glycation of key macromolecules or basement membrane components in individuals with diabetes, which may slow the formation of exfoliation material, the authors noted.
“Interestingly,” they wrote, one transmission electron microscopy study of anterior lens epithelial cells found that the XFS in those with diabetes “presented with less intense modifications on the lens and a better-conserved epithelium” compared to XFS patients without the condition. “This underscores the importance of continuing the efforts to elucidate the disease mechanism of XFS and the etiology of abnormal accumulation of fibrillin material.”
The authors noted that these findings should be interpreted with caution due to the substantial heterogeneity and marginally significant publication bias across the studies. At the same time, these findings provide a basis for future research to confirm these findings with larger-scale, longitudinal epidemiological data and correlation with objective markers of diabetes disease severity and progression such as HbA1C.
Future research should consider more large-scale prospective cohort studies that incorporate gene-environment interactions as well as studies that rely less on self-report of diabetes and more objective, standardized definitions (e.g., HbA1c, fasting glucose), the authors suggested in their journal article.
“Searching for a potential association between XFS and other systemic diseases may provide important new insight into the potential treatment and management of XFS,” they concluded.
Yu M, Hwang HH, Wiggs JL, et al. Association between diabetes and exfoliation syndrome: a systemic review and meta-analysis of observational studies. Ophthalmology Science. November 13, 2023. [Epub ahead of print.] |

