 History
History
A 37-year-old black male was referred for an emergency eye examination following an allergic reaction to an oral antibiotic. His ocular complaints included mild blurry vision, red eyes and pain; the symptoms were worse in his left eye. His systemic history was positive for HIV.
Diagnostic Data
His best-corrected acuity was 20/30 O.U. The external examination was normal, and there was no evidence of afferent pupillary defect.
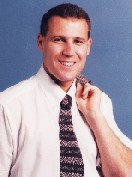
Refraction revealed mild myopia. The patients ocular and facial appearance is illustrated in the photograph. Intraocular pressure measured 12mm Hg in both eyes. Dilated fundus exam was normal in both eyes.
 Your Diagnosis
Your Diagnosis
How would you approach this case? Does this patient require any additional tests? What is your diagnosis? How would you manage this patient? What is the likely prognosis?
Discussion
The diagnosis in this case is Stevens-Johnson syndrome (SJS), sometimes referred to as erythema multiforme major.
SJS is an acute, self-limited, nonprogressive inflammatory disorder of the skin and mucous membranes. The minor form of erythema multiforme primarily affects the skin and lasts two to three weeks. The Stevens-Johnson variant is more serious, and is characterized by skin lesions and erosion of mucous membranes. These symptoms can last up to six weeks. Other symptoms include malaise, fever, headache and denudation of the epidermis.
SJS typically affects healthy young people within the first three decades of life. However, the condition can also affect people of all ages. It often is more prevalent in males than females. The disease can be fatal.
While the exact cause is unknown, numerous antigens precipitate SJS. These include bacteria (Mycoplasma pneumoniae), viruses (herpes simplex virus), fungi and drugs (sulfonamides, penicillin, barbiturates, salicylates, mercurial agents, arsenic, phenylbutazone, phenytoin, topical scopolamine, tropicamide and proparacaine). SJS may occur secondary to neoplasms, radiation therapy, collagen vascular diseases, various vaccinations, and as an idiopathic reaction to some medications. Genetic associations include HLA-Bw44 and HLA-B12.
The histologic changes in erythema multiforme suggest an underlying vasculitis or perivasculitis. Mononuclear cells, eosinophils and polymorphonuclear neutrophil leukocytes occur around the vessels or within the vessel wall, causing fibrinoid necrosis.
Erythema multiforme major often begins with symptoms of malaise, fever and headache. Next, skin lesions develop symmetrically on the extremities or face. The skin lesions are round, erythematous macules that develop into papules, and then into vesicles or bullae. Eventually, the bullae rupture, causing epidermal necrosis. The lesions appear red-centered, surrounded by a pale zone and an outer red ring. If extensive skin necrosis occurs, the condition is labeled toxic epidermal necrolysis.
The extent of both mucous membrane and skin involvement is usually congruent. The mouth and eyes are affected most frequently and severely. In one study, 100% of patients had stomatitis, and 63% had conjunctivitis.
Patients with ocular involvement may develop an acute, bilateral, mucopurulent conjunctivitis. Those severely affected develop chemosis, vesicles, bullae, pseudomembranes and corneal ulcerations.
The most serious ocular ailments occur when the disease enters the cicatricial stage. Despite all supportive measures, conjunctival scarring and symblepharon may still occur. Destruction of the conjunctival goblet cells, lacrimal gland and accessory lacrimal gland results in a pathologically dry eye. Other complications, such as entropion or trichiasis, can combine with the dry eye to produce corneal ulceration, vascularization, opacification and perforation.
Treatment options vary depending on the severity of the condition. Local treatment always involves lubrication of the ocular surfaces. Unfortunately, local treatment of the acute condition may have little influence on the severity of the cicatricial complications. Consider prescribing an oral corticosteroid, such as prednisone 60mg to 80mg per day. Conjunctivitis should be treated if present; but do not use an antibiotic, such as penicillin, that could stimulate the current toxic reaction.
Surgery, such as conjunctival or eye lid reconstruction, can be ordered to correct complications of entropion and trichiasis induced by scarring. Finally, conjunctival, amniotic or buccal mucous membrane grafts, along with stem cell transplantation, can be considered to restore the ocular surface.
In this case, the patient was treated with oral steroids, antihistamines, soothing lotions and other palliative approaches. Recovery was slow, yet eventual, lasting four to six weeks.

