 |
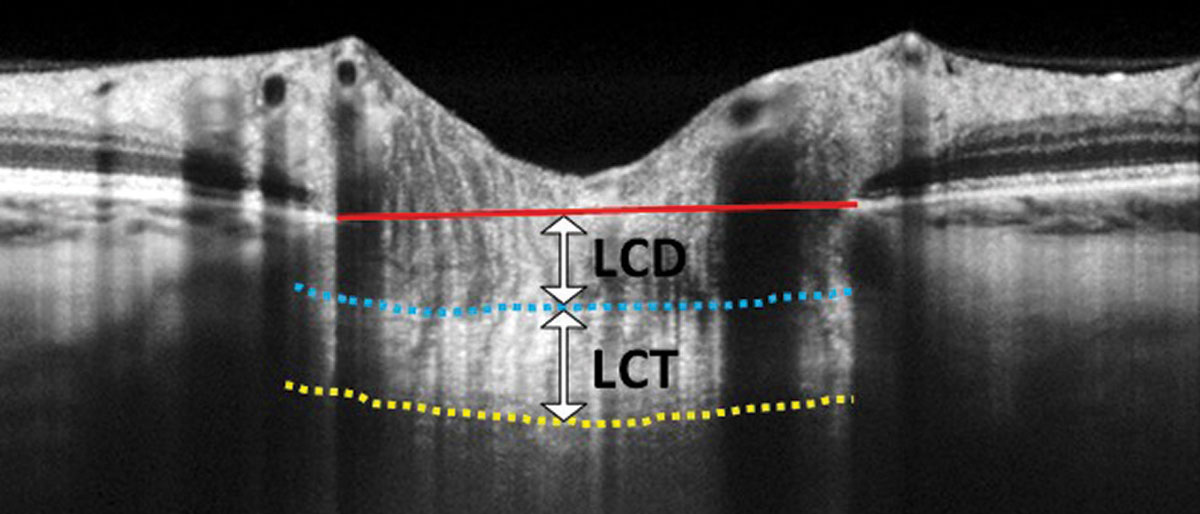
In this EDI-OCT through the optic nerve, the lamina cribrosa thickness (LCT) is measured from the anterior border (blue dashed line) to the posterior border (yellow dashed line). Lamina cribrosa depth (LCD) is measured along a perpendicular line from the anterior border of the lamina to a reference line that connects the edges of Bruch’s membrane (red solid line). Photo: Carolyn Majcher, OD. Click image to enlarge. |
One of the major diagnostic challenges faced by clinicians is differentiating glaucomatous myopes from myopes with glaucoma-mimicking visual defects. As the number of individuals with myopia and high myopia increases each year, this need to distinguish the two conditions will only increase. Clinicians typically rely on optic nerve findings and visual field progression monitoring to make the call. A study published last Friday in the Journal of Glaucoma investigated in vivo lamina cribrosa characteristics in high myopes with and without open-angle glaucoma. While both conditions entail lamina cribrosa thinning, researchers found significant differences between the degree of thinning in high myopia and open-angle glaucoma compared with high myopia alone.
The study included 240 highly myopic eyes (axial length ≥ 26mm), 46 of which had open-angle glaucoma. Using OCT and OCT-A, the researchers assessed the following: lamina cribrosa center, externally oblique border, an abrupt change of scleral curvature (scleral step), deep-layer microvasculature dropout and global RNFL thickness.
The researchers reported that highly myopic glaucomatous eyes had significantly thinner lamina cribrosa than highly myopic eyes alone (107.76µm vs. 137.01µm). High myopia alone was associated with deep-layer microvasculature dropout as well as elevated IOP.
Using the lamina cribrosa to detect open-angle glaucoma demonstrated an area under the curve (which measures the strength of correlation) of 0.964, a statistically higher value than detection based on global RNFL thickness (0.921) and vertical cup-to-disc ratio (0.902). The researchers reported that a lamina cribrosa thickness cut-off value of 128µm produced 100% sensitivity and 84% specificity for detecting open-angle glaucoma.
Eyes with high myopia demonstrated reduced lamina cribrosa center thickness and an abrupt change in scleral curvature with larger externally oblique border distance, but interestingly, lamina cribrosa thinning wasn’t associated with axial length elongation.
“Further thinning of the lamina cribrosa center in highly myopic open-angle glaucoma was associated with elevated intraocular pressure and the presence of microvascular dropout,” they wrote in their paper on the work. “Thinning of the lamina cribrosa center suggested a potential accuracy for open-angle glaucoma diagnosis in high myopia.”
They concluded that clinicians “should carefully consider the presence of glaucomatous optic neuropathy in eyes with a thickness of ≤128µm in the lamina cribrosa center.”
Chen Y, Mi B, Li H, et al. Thinning of the lamina cribrosa and deep layer microvascular drop out in patients with open angle glaucoma and high myopia. J Glaucoma. April 14, 2023. [Epub ahead of print]. |

