 |
Q:
I have a 39-year-old patient who went in for a fractured ulna repair under general anesthesia with a nerve block. When he woke up from surgery, he had a unilateral ptosis and miosis on the same side as the surgical arm. Both findings resolved completely within three to four days. What is going on?
A:
“Although seemingly innocent, ptosis and miosis are classic signs of Horner’s syndrome,” says Kristen Thelen, OD, of Emory Eye Center in Atlanta. “These findings can be indicators of more insidious underlying conditions.”
When a ptosis is present with miosis, it is a sign of a disruption within the sympathetic nervous system (SNS). In this case, it appeared to be an inconsequential side effect of the anesthesia. It is a surprisingly common complication with certain types of nerve blocks.
However, according to Dr. Thelen, knowing the pathway of the SNS is crucial for identifying other underlying causes of Horner’s syndrome and gauging the severity of your patient’s situation. Considering the associated nerve block and lack of additional central nervous system involvement, this patient likely had a disruption within the third-order neuron pathway.
The third-order neurons are located near the stellate ganglion and great vessels of the neck. Simply because of proximity, the third-order neurons are vulnerable to the effects of anesthesia. When blocks are administered in the neck area, the anesthesia can temporarily affect the adjacent third-order neurons. It’s likely that a supraclavicular approach was used to deliver the nerve block for the patient’s arm surgery.
First-order and second-order neuron involvements often occur from brain or spinal cord damage but was thankfully not the case in this patient. Had here been any concern for first- or second-order neuron involvement, imaging of the entire three-neuron sympathetic pathway would have been necessary.
 |
Horner’s syndrome after nerve block. Click image to enlarge. |
Anatomy and Differentials
The etiology of Horner’s syndrome can be classified by the anatomical location of sympathetic disruption. Here are some examples of conditions that can result in Horner’s syndrome based on first-, second- or third-order neuron disruption:
First-order neuron: hypothalamus to ciliospinal center of Budge.
• Multiple sclerosis
• Cerebral vascular accident (CVA)
• Spinal trauma above the T2 to T3 level
• Spinal cord tumor
Second-order neuron: T1 level of the spinal cord to C3 to C4.
• Tumor involving apex of the lung
• Lesions of the subclavian artery (an aneurysm)
• A dental abscess involving the mandibular region
Third-order neuron: external carotid to trigeminal nerve.
• Carotid cavernous fistula
• Internal carotid artery dissection or an aneurysm
• Cluster headaches or migraines
• Herpes zoster infection
• Temporal arteritis
• Local anesthesia
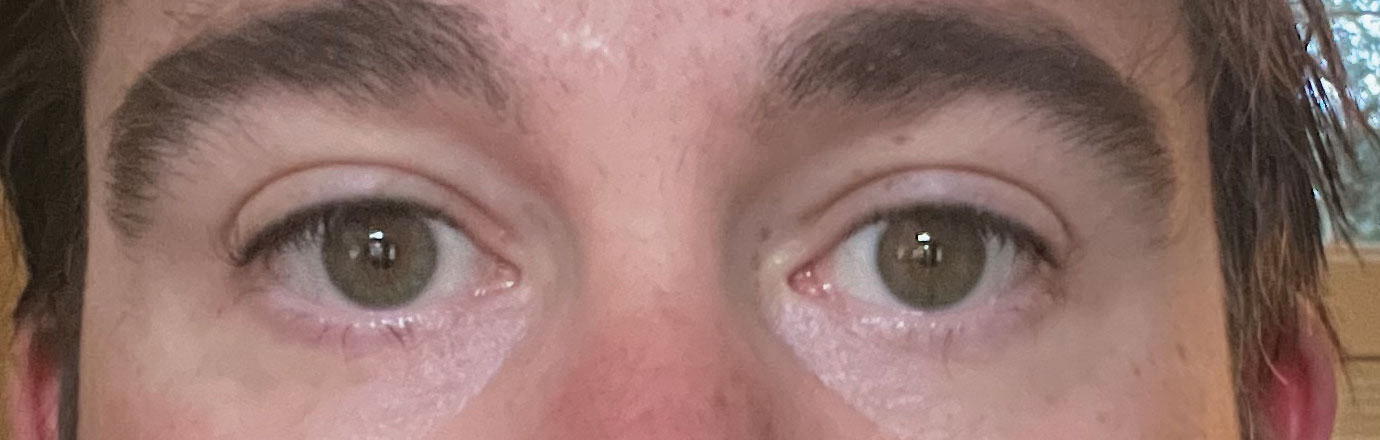 |
An almost complete resolution after four days. Click image to enlarge. |
Testing
Cocaine and hydroxyamphetamine are the standard agents used in diagnostic testing for patients with Horner’s syndrome. Due to cost and security concerns, these drugs are not widely available and are not realistic for most clinic settings. Apraclonidine is widely available and a great diagnostic tool for confirming your diagnosis, but it will not provide the location of the SNS lesion. When topically applied in Horner’s syndrome, apraclonidine will cause dilation of the affected pupil and no change to the normal pupil.
“Once your diagnosis of Horner’s is confirmed, and you’ve taken a detailed history from your patient, you can make a better decision on imaging timeline,” Dr. Thelen says. “In the rare case of acute, painful Horner’s (i.e., neck pain), this should be considered a neurological emergency because of the risk for dissection of the internal carotid artery.”
Prognosis
Based on the lack of additional neuro symptoms and speedy resolution of this patient’s Horner’s syndrome, Dr. Thelen suggests that they likely had a heavy dose of anesthesia administered during their nerve block. This could have easily caused a temporary and isolated disruption in the sympathetic cervical chain.
A study published on the National Institutes of Health’s website reports the incidence of a temporary Horner’s in 100% of the patients with an interscalene block of the brachial plexus.1 An interscalene block is a type of supraclavicular block often used in orthopedic medicine. “Temporary Horner’s cases are not uncommon with anesthesia, and they are usually no cause for alarm,” she notes.
Irrespective of the etiology, some patients with Horner’s have permanent sequelae. If symptoms are bothersome enough to cause quality-of-life or cosmetic concerns, there are pharmacological and surgical treatment options. The ptosis can be treated medically with Upneeq 0.1%(oxymetazoline hydrochloride ophthalmic solution, RVL Pharmaceuticals) or surgically by an oculoplastics specialist.
Dr. Ajamian is board certified by the American Board of Optometry and serves as Center Director of Omni Eye Services of Atlanta. He is vice president of the Georgia State Board of Optometry and general CE chairman of SECO International. He has no financial interests to disclose.
1. Walid T, Mondher BA, Mohamed Anis L, Mustapha F. A case of Horner’s syndrome following ultrasound-guided infraclavicular brachial plexus block. Case Rep Anesthesiol. 2012;2012:125346. |

