 |
|
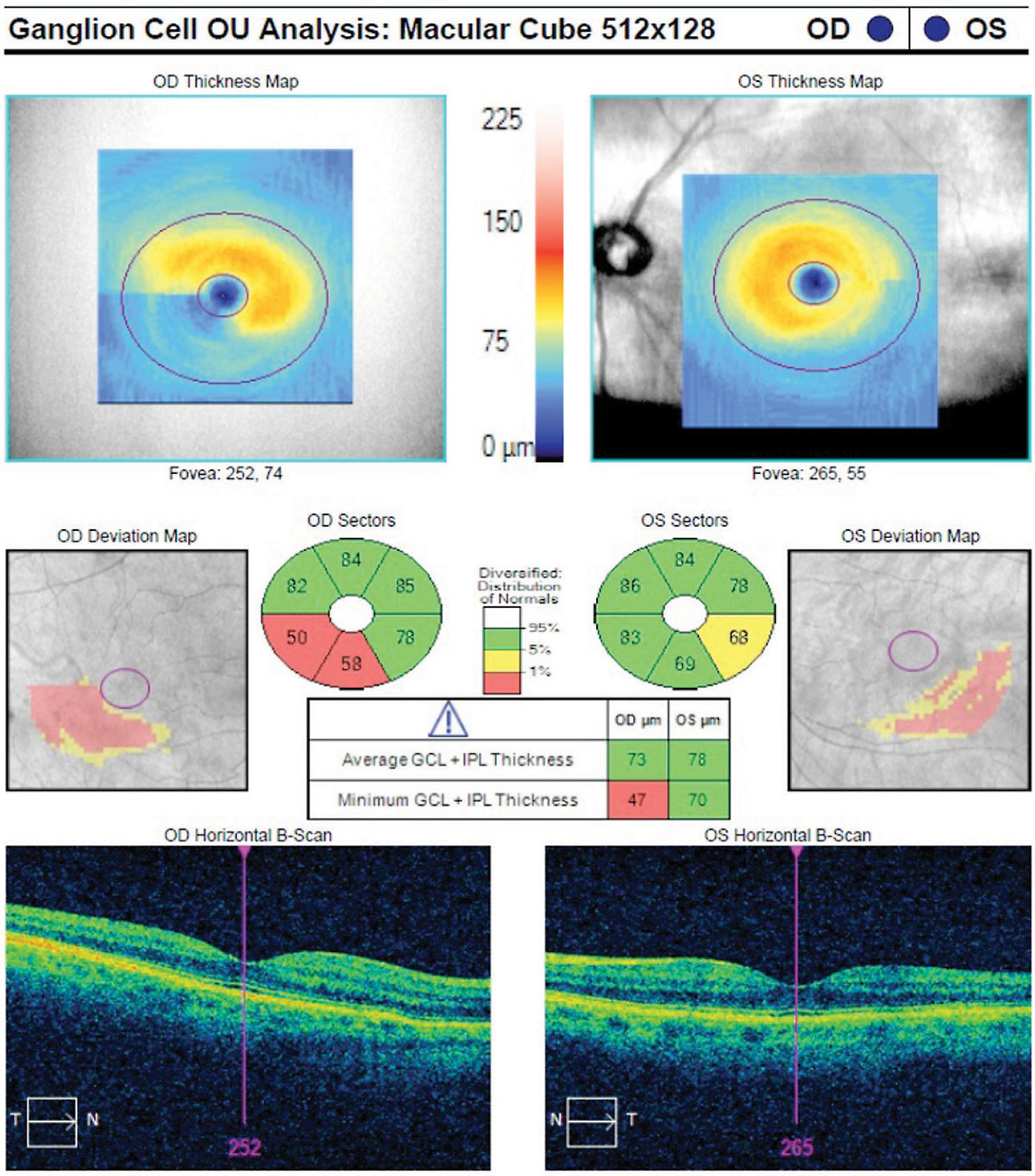
GCIPL thinning shown on macular OCT was found in this study to correlate with increased disease risk in glaucoma suspects. Photo: Danica Marrelli, OD. Click image to enlarge. |
As the researchers of a new study appearing in JAMA Ophthalmology explain, vulnerabilities in the macular and peripapillary areas are fertile ground for the development of diagnostic tests for perimetric glaucoma risk.
Data was collected from a tertiary center study and multicenter study, with participants with suspected glaucoma followed up for 3.1 years. Perimetric glaucoma was defined as three consecutive results showing abnormal visual fields. The researchers developed a model to investigate how performance of ganglion cell/inner plexiform layer (GCIPL) and circumpapillary retinal nerve fiber layer (cpRNFL) rates of thinning predict developmental risk for perimetric glaucoma.
Of the 462 participants (60% female) and 658 eyes, 23% developed perimetric glaucoma. GCIPL thinning rates were faster in eyes that did develop the condition. Every one µm/y faster rate of minimum GCIPL was associated with a 2.4 higher risk rates of developing this subset of glaucoma, while global cpRNFL thinning rates were associated with a 1.9 higher risk rate. Predictive factors of developing perimetric glaucoma included African American race, male sex, 1-dB higher baseline visual field pattern standard deviation and 1mm Hg higher mean intraocular pressure during follow-up.
The amount of IOP-lowering medications used in those with suspected glaucoma that did go on to develop perimetric glaucoma was much higher than those that did not, the researchers of the study note. As such, more intensive treatment of these cases is not enough in this group of patients even with sufficient follow-up time.
Previous research shows similar GCIPL thinning in early glaucoma eyes with faster thinning in more severe stages. Because of this, the researchers of the study propose that “evaluation of macular GCIPL in eyes with suspected glaucoma may be considered for monitoring these patients with suspected glaucoma, and it is worth performing macular scans for all patients with glaucoma.”1
The study likewise reflects prior research that has established African Americans experience a higher incidence of glaucoma. Because of their own findings and established literature, they suggest “African American patients with suspected glaucoma require close monitoring for timely detection of the development of perimetric glaucoma.”1
Also published in JAMA Ophthalmology was a commentary on the study’s results outlining how OCT has changed the way glaucoma is diagnosed.
The author, Joel S. Schuman, MD—one of the founding fathers of OCT use in eye care—explains that the invention of OCT caused interest in diagnosing glaucoma through cpRNFL and optic nerve head parameters due to its higher axial resolution of about 10µm.
The reasoning went that the cpRNFL would provide better assessment of glaucoma damage because it offers a better representation of the entire eye. Macular thickness turned out to be a good measure of glaucoma presence or absence, and measures that allow quantification of the macula’s layers, like the GCIPL, resulted in better discrimination of glaucoma than macular total retinal thickness.
He then explains that the authors of the study, rather than detecting the presence or absence of disease, actually looked at future progression risk to perimetric glaucoma. The author of the commentary highlights that the original study authors think that ONH and macular OCT imaging should be considered when managing suspected glaucomatous eyes. He ends with the point that “the literature is clear in light of this and prior studies demonstrating the value of macular OCT in the detection of glaucoma, the longitudinal assessment of glaucoma and the prediction of glaucoma progression.”2
1. Mohammadzadeh V, Moghimi S, Nishida T, et al. Association of rates of ganglion cell and inner plexiform thinning with development of glaucoma in eyes with suspected glaucoma. JAMA Ophthalmol. March 2, 2023. [Epub ahead of print]. 2. Schuman JS. Macular optical coherence tomography—from diagnosis to prognostication. JAMA Ophthalmol. March 2, 2023. [Epub ahead of print]. |

