23rd Annual Glaucoma ReportFollow the links below to read the other articles from our 23rd annual Glaucoma Report:Glaucoma Surgery: Are You Ready to Refer? Looking to the Future of Glaucoma Treatment Mastering MIGS: Today and Tomorrow |
Advancing technology has revolutionized our toolbox for detecting and following glaucoma progression—but knowing which tests provide the best diagnostic information is trickier than ever. Although 24-2 and 30-2 perimetry remain the gold standard—despite advancements in retinal nerve fiber layer (RNFL) and ganglion cell analysis (GCA) optical coherence tomography (OCT)—it may not be the most sensitive test to catch patients at the highest risk of functional visual impairment.1,2 Central 10-2 visual field (VF) testing, however, may be under-used in all stages of glaucoma.
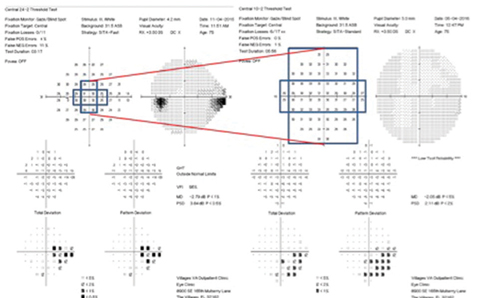 |
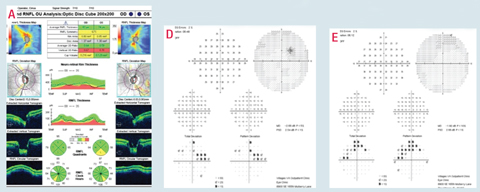
| Fig. 1. As this comparison shows, 10-2 perimetry has greater sensitivity and detects more points than 24-2 perimetry. |
These glaucoma cases—incorporating 10-2 and 24-2 perimetry, RNFL and GCA OCT and optic nerve head photos—highlight the benefits of 10-2 perimetry in detecting paracentral and VF defects close to fixation in all stages of glaucoma, with special attention to the early-moderate stage. In addition, these cases also suggest the benefits of using 10-2 VF testing to monitor progression and change in advanced visual field loss.
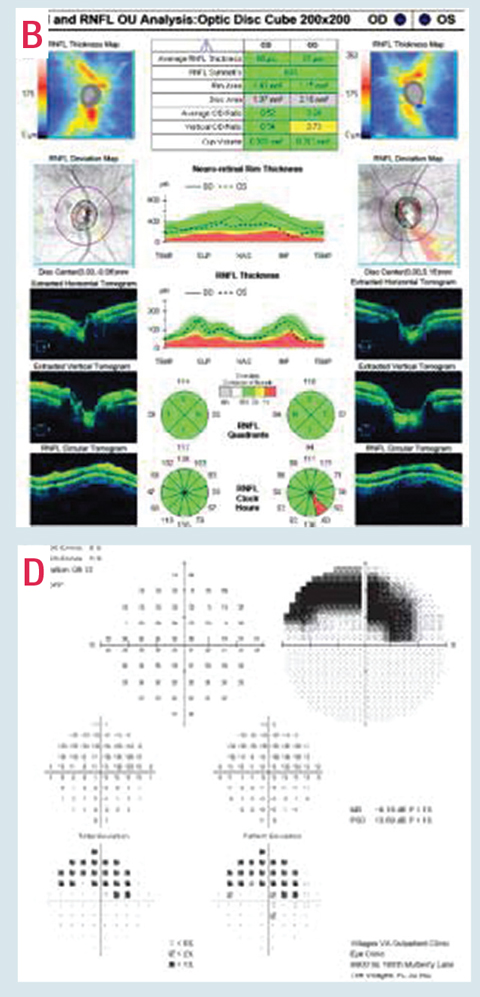
Case 1This 76-year-old patient has early-moderate primary open-angle glaucoma in the left eye and is a high-risk glaucoma suspect in the right. His IOPs were stable with current topical ocular hypotensive medications. Gonioscopy was normal OU and pachymetry measurements were thinner than average, 504μm OD and 508μm OS. Despite limited commitment to follow-up, his most recent 24-2 for his left eye (B) confirmed overall stable superior paracentral defects, which were consistent with inferior neuroretinal rim thinning (A) and moderate inferior/inferior-temporal RNFL loss on OCT testing (C). The patient’s current 24-2 test pattern isn’t sufficient to fully understand his level of visual impairment and reliably monitor for glaucomatous progression. Central 10-2 testing (D), however, can help reveal the risk of potential visual impairment and better monitor for disease progression. Click images to enlarge. | 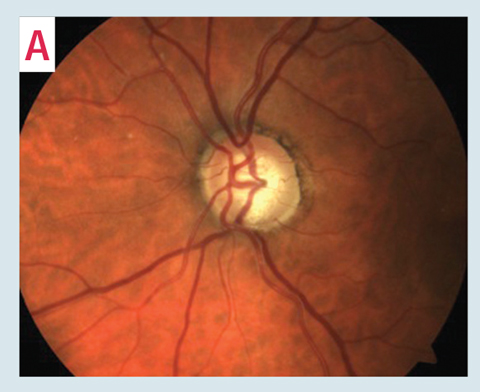 |
 | |
Why 10-2?
The 24-2 and 30-2 threshold VF testing patterns assess a total of 54 and 74 points, respectively, each six degrees apart (three degrees from the horizontal and vertical meridians) with only 12 points tested within the central 10 degrees (Figure 1). Furthermore, only four of these points are actually tested within the macular region (the central eight degrees)—the area that accounts for over 30% of the total retinal ganglion cells and over 60% of the visual cortex area.3
By comparison, 10-2 threshold VF testing assesses 68 points, more than five times as many points in the central 10 degrees compared with 24-2 and 30-2 testing. These points are all two degrees apart, just one degree from either side of the horizontal and vertical meridians.4 As a result of this greater sensitivity, many paracentral scotomas involving only a small area of the visual field at or near fixation may be missed with 24-2 and 30-2 perimetry and are only detected with 10-2 testing.5
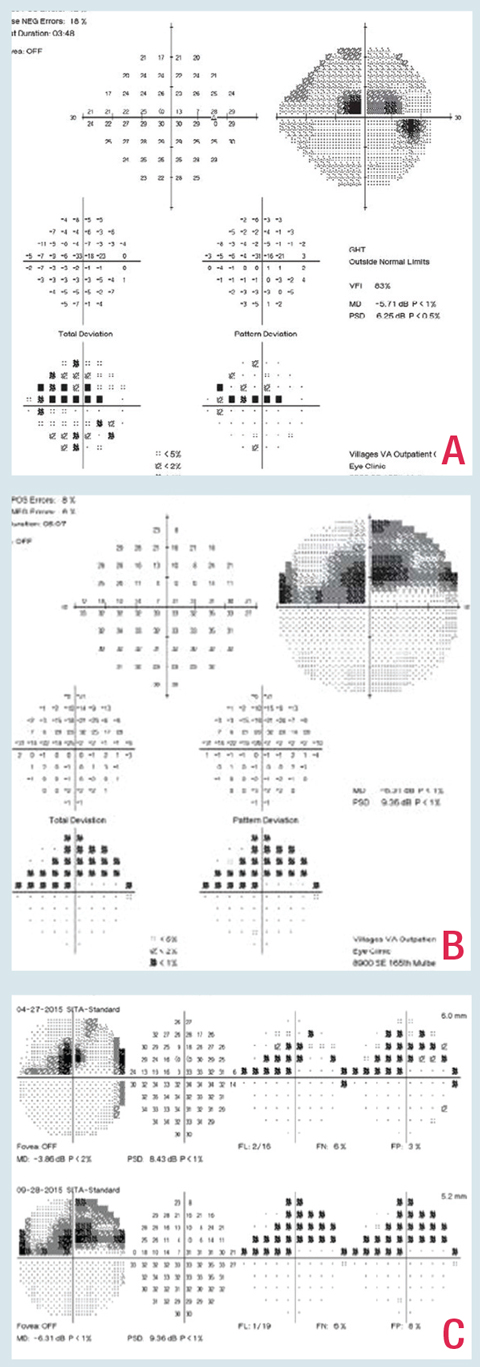
Case 2This patient’s 24-2 VF testing shows apparent advanced structural and functional glaucomatous damage with diffuse and deep superior central and paracentral damage (A). Such testing alone can lead clinicians to not only underestimate the extent of glaucomatous VF damage, but also overestimate the extent of damage and potentially miss the area of remaining superior temporal paracentral sensitivity (B). Click images to enlarge. |
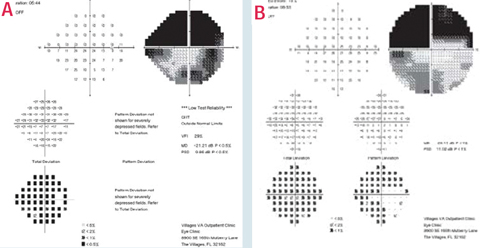 |
Case 3This patient has detectable rim loss upon optic nerve evaluation and OCT testing (A) with correlating nasal step visual field defects OU, more so in the right eye than the left, and presumed minimal central involvement on visual field 24-2 testing, again more so in the right eye than the left (B and C). Central 10-2 visual field testing shows that 24-2 testing underestimates these potential central defects (D and E). Click images to enlarge. | 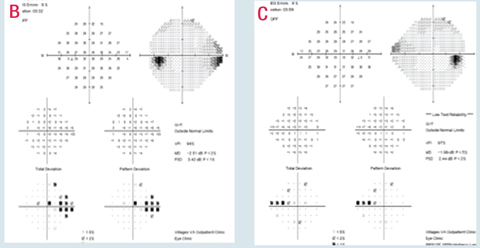 |
 | |
Early and Moderate Glaucoma
Although central and paracentral glaucomatous VF damage more commonly occurs in advanced stages of glaucoma, such defects also occur in patients with earlier stages of glaucoma and with relatively minimal peripheral VF loss.6 Recent studies suggest these early central defects are usually more common in the upper VF, deeper and generally have an arcuate-like pattern that is closer to fixation than those in the inferior VF.7
Central and paracentral defects in patients with early or moderate glaucoma are more common than you might expect. According to one study, more than 50% of eyes with mild-moderate glaucoma have such defects within the central three degrees.8 Furthermore, research suggests macular damage evidenced on GCA OCT, with correlating functional damage on 10-2 testing, occurs almost as frequently as peripheral defects in patients with early glaucoma; approximately 16% of these patients may have undetected functional central defects when using 24-2 testing alone.4,9 Another study found 9% of normal 30-2 threshold VFs in glaucoma suspects or early glaucoma patients were actually classified as abnormal with 10-2 testing.10 Additionally, 30-2 underestimated the level of glaucomatous damage in 13% of the hemifields.10 Other researchers found 11 eyes with normal 24-2 VFs outside the central 10 degrees showed arcuate defects within the central 10 degrees with 10-2.11
In a study published online May 24, 2017, researchers found that, in cases of normal 24-2 testing, 10-2 found abnormal central defects in 35% of the patients with ocular hypertension, 39% of glaucoma suspects and 61% of the patients with early glaucoma.12 An abnormal 10-2 result was significantly associated with at least one location on the total deviation or pattern deviation plot (p <0.5%) within the central 10 degrees on 24-2 testing.12 They also found patients of African descent were more likely to have central VF defects.12
Key point: Armed with such evidence, one group of researchers recommends 10-2 VF testing always be considered if: there are any depressed points in the central 12 degrees less than 0.5% on 24-2 or 30-2 VF testing; the paracentral defect is greatly depressed relative to the mean deviation (MD) on 24-2; or there are any abnormal points in the central 12 points on 24-2 testing that spatially correlate to thinning in the macular ganglion cell inner plexiform layer (GCIPL) area.13
Case 4This patient has superior rim thinning (A and B) with correlating RNFL loss on OCT testing (C and D). This corresponds to associated inferior paracentral and nasal visual field defects with variable central defects in both eyes (D and E). Due to these borderline defects and the spatially correlating ganglion cell complex thinning in the left eye (F), central 10-2 visual field testing better documented the breadth and depth of these defects (G and H). Click images to enlarge. | 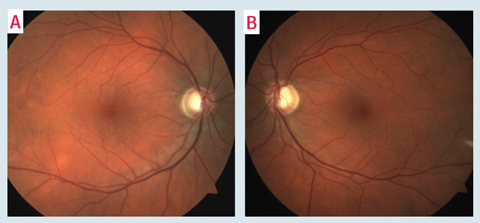 |
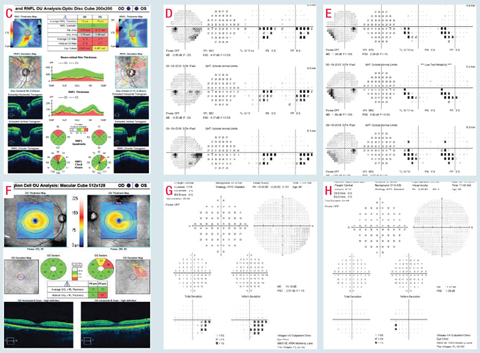 | |
Case 5Despite relatively mild inferior temporal neuroretinal rim loss in this patient’s right eye (A) with confirmed RNFL loss on OCT (B), and regardless of the status of the rest of the visual field, this patient has advanced visual field loss on 24-2 visual field testing (C). Due to this deep central involvement, 10-2 visual field testing is critical to better understand the significance of this defect and monitor for progression (D). Click images to enlarge. | |
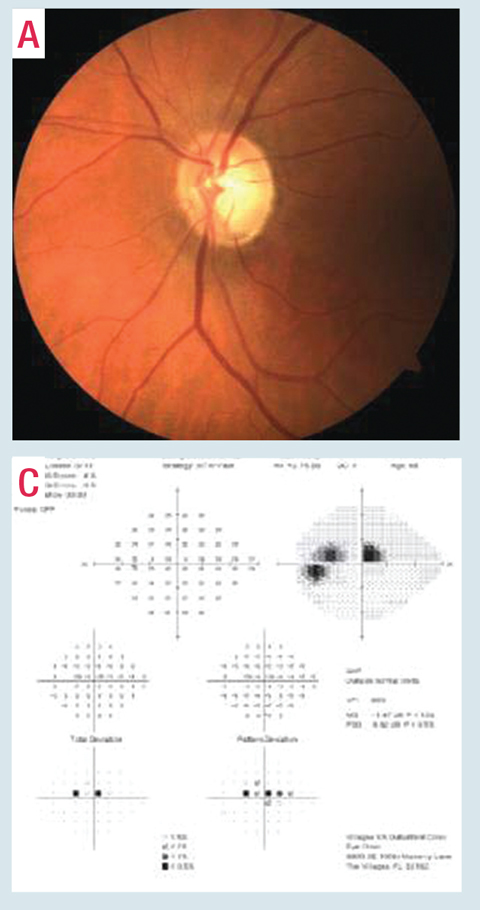 |  |
Advanced Glaucoma
According to the Hodapp, Parrish, and Anderson visual field classification system, one of the criteria for advanced glaucoma is if the VF has any points within the central five degrees with a sensitivity less than or equal to 0dB, or if both hemifields have depressed points with sensitivity less than 15dB within the central five degrees of fixation—regardless of the status of the rest of the visual field.14 For these patients in particular, and even for patients with good central visual acuities, clinicians should regularly use 10-2 testing to better understand the significance of the defect and better monitor for progression.15,16 Furthermore, researchers highly recommend all patients with advanced glaucoma undergo a combination of 24-2 or 30-2 and 10-2 testing as close to one another as possible, or at least alternated at future follow-up visits, to help monitor for progression.6
Case 6This patient presented with severe inferior temporal glaucomatous structural damage and has a corresponding superior central and paracentral 24-2 VF defect (A). Central 10-2 testing reveals the extent of this defect and better highlights the possible progression that likely would have been underestimated or missed on 24-2 testing alone (B and C). Click images to enlarge. |
 |
For advanced cases, several studies have found that 10-2 testing with non-standard V size stimulus (as opposed to the standard III size stimulus) can more reliably measure visual function that was otherwise undetected on 30-2 testing with standard III size and thus help monitor progression of points with lower sensitivity for a longer period.17,6
Glaucoma Progression
Early evidence-based research shows 10-2 perimetry detects central and paracentral glaucomatous progression more frequently than 24-2 VF testing.18 In addition, one study found the rate of MD change was similar on 24-2 and 10-2 VF testing with mild to moderate VF loss, but the rate of MD change was significantly greater on 10-2 compared with 24-2 testing for eyes with advanced VF loss (-0.19dB/year for 24-2 testing and -0.26 dB/year for 10-2 testing).15
By using central 10-2 VF testing more routinely, clinicians can hopefully diagnose glaucoma earlier, detect progression sooner and minimize the risk of under- or overestimating the extent of the glaucomatous visual field damage—in all stages of glaucoma.
Drs. Lifferth, Fisher, Cordes, Carter and Perkins are attending optometrists at The Villages VA Outpatient Clinic, in Fla.
Dr. Stursma is an attending optometrist at the Ocala Community Based VA Outpatient Clinic in Ocala, Fla.
| 1. Khoury J, Donahue S, Lavin P, Tsai J. Comparison of 24-2 and 30-2 perimetry in glaucomatous and nonglaucomatous optic neuropathies. J Neuroophthalmol. 1999;19(2):100-8. 2. Heijl A, Bengtsson B, Chauhan B, et al. A comparison of visual field progression criteria of 3 major glaucoma trials in early manifest glaucoma trial patients. Ophthalmology. 2008;115(9):1557-65. 3. Schira MM, Wade AR, Tyler CW. Two-dimensional mapping of the central and parafoveal visual field to human visual cortex. J Neurophysiol. 2007;97(6):4284-95. 4. Traynis I, de Moraes CG, Raza AS, et al. Prevalence and nature of early glaucomatous defects in the central 10 degrees of the visual field. JAMA Ophthalmol. 2014;132(3):291-97. 5. Hangai M, Ikeda H, Akagi T, et al. Paracentral scotoma in glaucoma detected by 10-2 but not by 24-2 perimetry. Jpn J Ophthalmol. 2014;58(2):188-96. 6. de Moraes C, Liebmann J, Medeiros F, et al. Management of advanced glaucoma: characterization and monitoring. Surv Ophthalmol. 2016;61(5):597-615. 7. Hood D, Slobodnick A, Raza A, et al. Early glaucoma involves both deep local, and shallow widespread, retinal nerve fiber damage of the macular region. Invest Ophthalmol Vis Sci. 2014;55(2):632-49. 8. Schiefer U, Papageorgiou E, Sample PA, et al. Spatial pattern of glaucomatous visual field loss obtained with regionally condensed stimulus arrangements. Invest Ophthalmol Vis Sci. 2010;51(11):5685-9. 9. Teixeira IC, Bresciani-Battilana E, Barbosa D, et al. Correlation between the ganglion cell complex and functional measures in glaucoma patients and suspects. Int Ophthalmol. 2015;35:81-7. 10. Langerhorst C, Carenini L, Bakker D, et al. Measurements for description of very early glaucomatous field defects. In: Wall M, Heiji A, eds. Perimetry Update 1996/1997. New York, NY: Kugler Publications;1997:67-73. 11. Hood DC, Raza AS, de Moraes CG, et al. Initial arcuate defects within the central 10 degrees in glaucoma. Invest Ophthalmol Vis Sci. 2011;52(2):940-6. 12. de Moraes C, Hood D, Liebmann J, et al. 24-2 visual fields miss central defects shown on 10-2 tests in glaucoma suspects, ocular hypertensives, and early glaucoma. Ophthalmology. May 24, 2017. [Epub ahead of print]. 13. Park H, Hwang B, Shin H, et al. Clinical clues to predict the presence of parafoveal scotoma on humphrey 10-2 visual field using a humphrey 24-2 visual field. Am J Ophthalmol. 2016 Jan;161:150-9. 14. Brusini P, Johnson C. Staging functional damage in glaucoma: review of different classification methods. Surv Ophthalmol. 2007;52(2):156-79. 15. Weinreb RN, Garway-Heath DF, Leung C, et al, eds. Progression of Glaucoma: The 8th Consensus Report of the World Glaucoma Association. Amsterdam: Kugler Publications; 2011:15. 16. Rao HL, Begum VU, Khadka D, et al. Comparing glaucoma progression on 24-2 and 10-2 Visual field examinations. PLoS One. 2015;10(5):e0127233. 17. Zalta A. Use of a central 10 degrees field and size V stimulus to evaluate and monitor small central islands of vision in end stage glaucoma. Br J Ophthalmol. 1991;75(3):151-4. 18. Park S, Kung Y, Ritch R, et al. Parafoveal scotoma progression in glaucoma: humphrey 10-2 versus 24-2 visual field analysis. Ophthalmol. 2013;120(8):1546-50. |

