 |
A 27-year-old Caucasian female presented to our emergency department with acute painless loss of vision in her left eye for 12 days. Five days prior to vision loss, she developed a fever, migraine, chills and myalgia. She initially presented to a local provider who referred her to a nearby emergency department, where she underwent extensive neuroimaging and serology testing.
Her past medical, ocular, social and family history were unremarkable. She was not taking any medications and had no known environmental or drug allergies. An extensive review of systems revealed recent weight loss attributable to her illness and exposure to her one kitten at home with no known bites or scratches.
Her visual acuity was 20/25 OD and 20/100 OS. Extraocular motilities and confrontation visual fields were full OU. Her pupils were equally round and reactive with no relative afferent pupillary defect, and her Ishihara color plates were full in OU. Intraocular pressures were 15mm Hg OD and 13mm Hg OS.
The patient’s anterior segment examination was unremarkable, notably with no anterior chamber cell or flare OU. Posterior segment contained rare vitreous cell OD and 1+ vitreous cell OS.
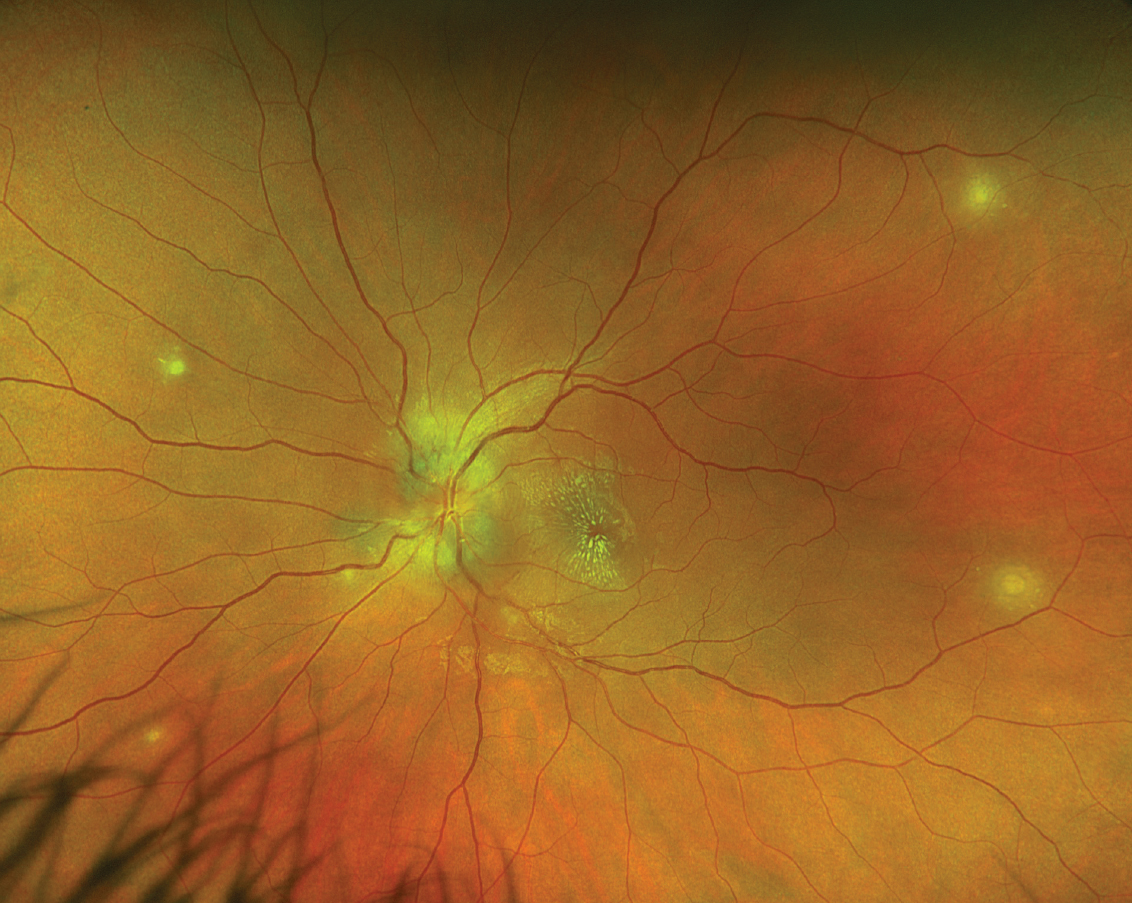
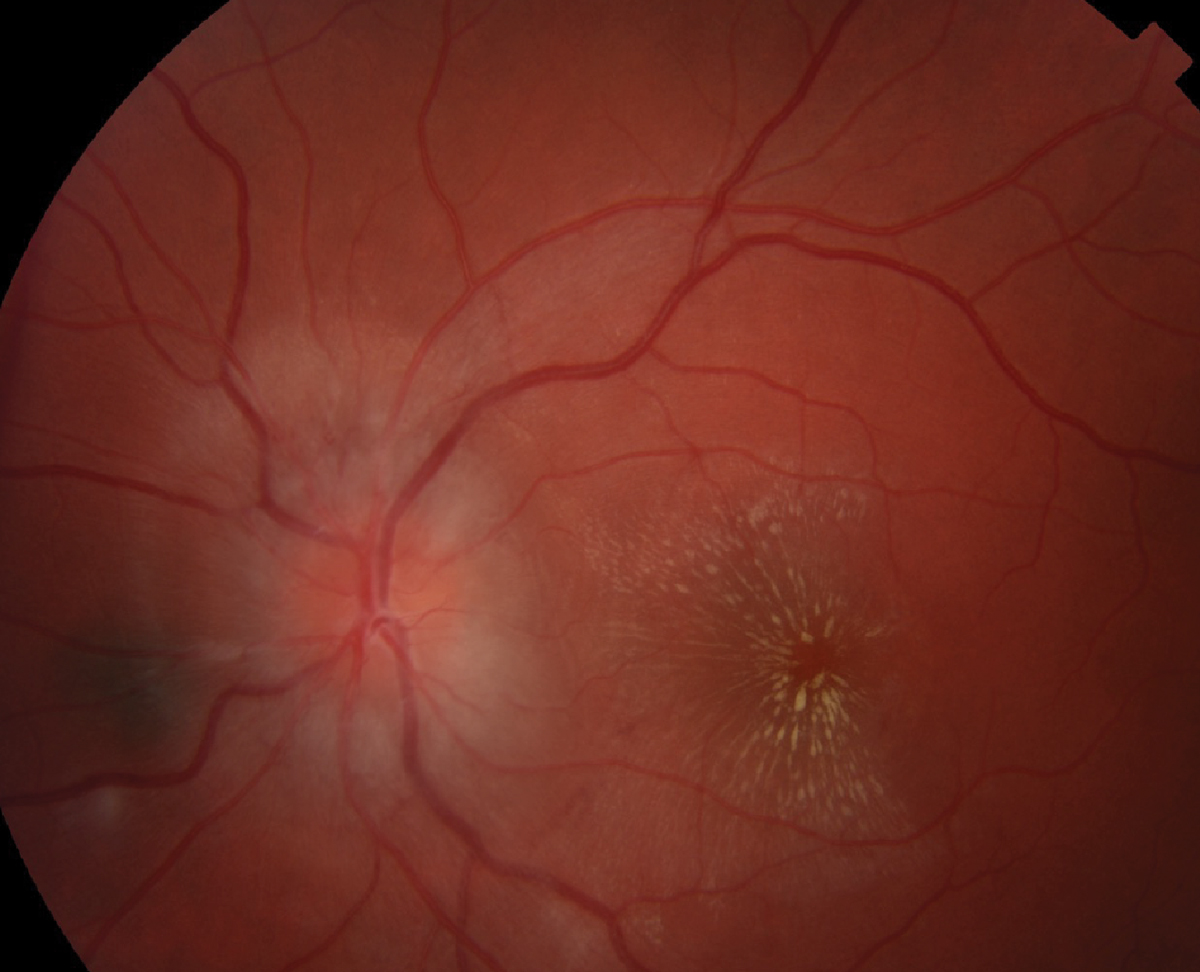
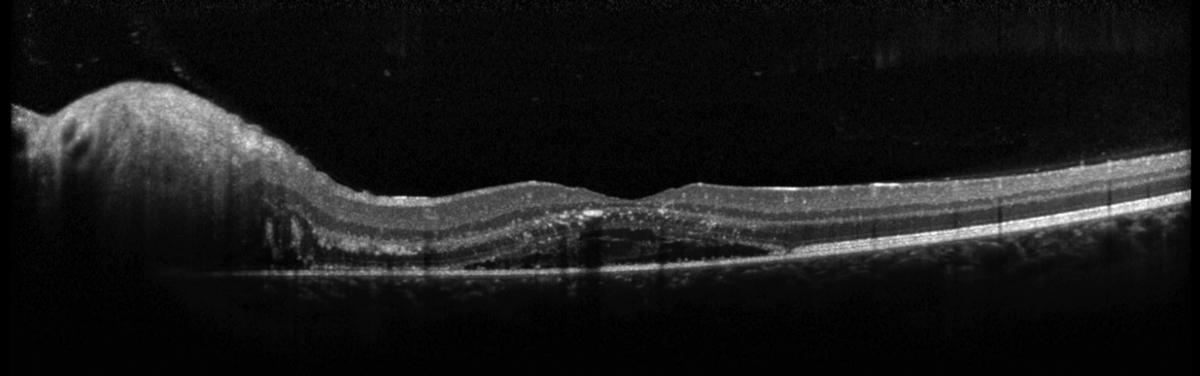
Fundus imaging and OCT are also available for review (Figures 1-4).
 |
|
Fig. 1. Optos widefield fundus photography of the right eye. Click image to enlarge. |
Take the Retina Quiz
1. Which of the following is true of the posterior segment imaging?
a. There is an exudative macular neovascular lesion in the left eye.
b. There is multifocal chorioretinitis in both eyes.
c. There is optic nerve edema in the right eye.
d. There is retinal vasculitis in both eyes.
2. What is the most likely diagnosis?
a. Cat scratch disease (CSD).
b. Diffuse unilateral subacute neuroretinitis.
c. Lyme disease.
d. Syphilis infection.
3. What organism is the cause of the suspected diagnosis?
a. Bartonella henselae.
b. Borrelia burgdorferi.
c. A nematode.
d. Trepnoma pallidum.
4. Which of the following is NOT a possible ophthalmic manifestation of the suspected organism?
a. Conjunctivitis.
b. Chorioretinitis.
c. Neuroretinitis.
d. All of the above are possible ophthalmic manifestations.
5. Which of the following is true?
a. The macular star is composed of a sub-RPE drusenoid material.
b. Gass first proposed that the macular serous detachment seen in neuroretinitis occurs secondary to leakage from the optic disc and should not be classified as a retinal vasculopathy.
c. Neuroretinitis should be treated empirically with oral valcyclovir if a viral-like prodrome precedes the presentation.
d. Surgical consult to oculoplastics should be considered on initial presentation for optic nerve sheath fenestration.
 |
|
Fig. 2. Optos widefield fundus photography of the left eye. Click image to enlarge. |
Diagnosis
Fundus exam revealed multifocal chorioretinitis OU (OS>OD) and optic nerve edema with macular star formation OS. The patient received an MRI scan of the brain and orbits with and without contrast as well as MRA and MRV of the brain without contrast at an outside hospital, all of which were normal.
Serology testing was significant only for Bartonella henselae IgG titer of 1:640 and IgM titer of 1:200. The patient was thought to have developed a bilateral posterior uveitis and unilateral neuroretinitis secondary to B. henselae infection.
Discussion
B. henselae is a gram-negative intracellular bacilli found worldwide responsible for cat scratch disease.1 Cats are the primary reservoir for B. henselae, and cat fleas are the main vector for transmission.1 Human infection occurs through scratches or bites that pierce the skin, or cat saliva on open skin lesions.1 Although they usually show no symptoms, 40% of cats carry B. henselae at some point in their lives with kittens younger than one year being more likely to have the infection and spread it to humans.2
Primary inoculation results in a local papule that develops within several days at the scratch site and is associated with regional lymphadenitis.3 Within a few weeks, disseminated infection may occur resulting in a “viral-like” prodrome consisting of fever, myalgia, chills, headache, malaise and weight loss.3 Bartonella infection is more common in children and young adults; immunocompromised patients may develop life-threatening complications such as endocarditis and encephalopathy.3
 |
|
Fig. 3. Topcon fundus photo of the posterior pole of the left eye. Click image to enlarge. |
Ocular involvement is seen in 5% to 10% of patients with CSD, and Bartonella remains the leading cause of neuroretinitis.4,5 In 5% of infections, the eye is the primary inoculation site and the individual may develop Parinaud’s oculoglandular syndrome, which is classically characterized as a unilateral follicular conjunctivitis with ipsilateral tender pre-auricular lymphadenopathy.4 Posterior ophthalmic manifestations of Bartonella include hypopigmented chorioretinal lesions (83%), optic disc edema (46%) and optic disc edema with macular star formation (43%).6
Interestingly, the white chorioretinal lesions are the most commonly seen posterior segment manifestation of Bartonella infection and are thought to represent choroiditis, inner retinitis or chorioretinitis that can be present even in the absence of neuroretinitis.6 These lesions fade slowly and result in chorioretinal atrophy.1
Neuroretinitis is an optic neuropathy characterized classically as a triad consisting of vision loss, optic disc edema and serous retinal detachment with the subsequent appearance of an exudative macular star. It was first described by Leber in 1916, who believed the etiology was retinal in nature; however, Gass later demonstrated that the maculopathy is actually secondary to vascular leakage in the optic nerve with the use of fluorescein angiography.7 The term “neuroretinitis” later became preferred for describing infectious causes of this presentation.7
B. henselae IgG tigers exceeding 1:256 are confirmatory.1 While mild CSD is typically self-limiting in an immunocompetent individual, neuroretinitis is a manifestation where treatment is indicated.1
 |
|
Fig. 4. Heidelberg OCT of the left macula. Click image to enlarge. |
There is controversy regarding the preferred antimicrobial agent as well as the use of systemic corticosteroids. Immunocompetent adults are typically prescribed doxycycline 100mg by mouth twice a day for two to four weeks.1 Longer treatment may be required in immunocompromised patients, and children may be prescribed azithromycin.1 A recent review suggests that patients with severe vision loss may have some benefit from four to six weeks of doxycycline combined with rifampin 300mg by mouth twice daily.8
The patient was made aware of the diagnosis and started on doxycycline 100mg twice daily for four weeks with close follow-up.
Retina Quiz Answers
1: b, 2: a, 3: a, 4: d, 5: b
Drs. Aboumourad and Black currently practice at Bascom Palmer Eye Institute in Miami. They have no financial disclosures.
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
1. Ksiaa I, Abroug N, Mahmoud A, et al. Update on Bartonella neuroretinitis. J Curr Ophthalmol. 2019;31(3):254-61. 2. Cat scratch disease (2020). Centers for Disease Control and Prevention. www.cdc.gov/healthypets/diseases/cat-scratch.html. Accessed: October 5, 2022. 3. Amer R, Tugal-Tutkun I. Ophthalmic manifestations of Bartonella infection. Curr Opin Ophthalmol. 2017;28(6):607-12. 4. Koretz ZA, Apostolopoulou A, Chen E, et al. Clinical features and multimodal imaging in atypical posterior uveitis secondary to Bartonella henselae infection. Ocul Immunol Inflamm. 2021;1-8. 5. Patel R, Patel BC, Chauhan S. Neuroretinitis. In: StatPearls. Treasure Island (FL): StatPearls Publishing. May 24, 2022. 6. Solley WA, Martin DF, Newman NJ, et al. Cat scratch disease: posterior segment manifestations. Ophthalmology. 1999;106(8):1546-53. 7. Brazis PW, Lee AG. Optic disk edema with a macular star. Mayo Clin Proc. 1996;71(12):1162-6. 8. Fairbanks AM, Starr MR, Chen JJ, Bhatti MT. Treatment strategies for neuroretinitis: current options and emerging therapies. Curr Treat Options Neurol. 2019;21(8):36. 9. Eyles DE, Coleman N. Antibiotics in the treatment of toxoplasmosis. Am J Trop Med Hyg. 1953;2(1):64-9. 10. Fernandes Felix JP, Cavalcanti Lira RP, Grupenmacher AT, et al. Long-term results of trimethoprim-sulfamethoxazole vs. placebo to reduce the risk of recurrent Toxoplasma gondii retinochoroiditis. Am J Ophthalmol. 2020;213:195-202. |

