 |
On ocular examination, his best-corrected visual acuity was 20/150 OD and 20/200 OS. Extraocular motilities were full, and confrontation visual fields were full to careful finger count in each eye. Pupils showed physiological anisocoria but no afferent pupillary defect. Intraocular pressures (IOP) were 14mm Hg OD and 12mm Hg OS.
Anterior segment evaluation revealed corneal arcus 360 OU. The anterior chamber in each eye was deep and quiet. In the right eye there was a posterior chamber intraocular lens, and the left eye had 3+ cortical, nuclear and posterior subcapsular cataracts. Posterior segment showed clear vitreous and healthy optic nerves in both eyes. In the right eye adjacent to the macula, an elevated, well-circumscribed lesion could be seen (Figures 1 and 2). Spectral domain ocular coherence tomography (SD-OCT) through the lesion (Figure 3) and a macular cube were also obtained (Figure 4). Posterior segment findings in the left eye were unremarkable.
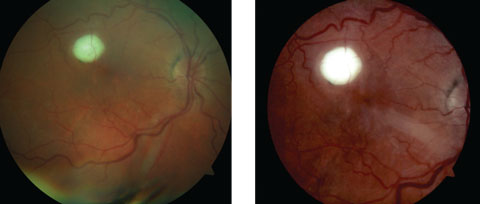 |
| Figs. 1 and 2. Both these fundus photos show our patient’s right eye. What does the lesion represent? Click image to enlarge. |
Take the Quiz
1. How would you characterize the lesion?a. Choroidal neovascular membrane.
b. Old macroaneurysm.
c. Posterior pole granuloma.
d. Chorioretinal coloboma.
2. What is the likely diagnosis?
a. Toxoplasmosis.
b. Choroidal osteoma.
c. Toxocariasis.
d. Ocular tuberculosis.
3. What is the OCT interpretation?
a. Hyper-reflective mass with RPE disruption.
b. Choroidal neovascular membrane.
c. Macular edema.
d. Both a and c.
4. How should this patient be managed?
a. Monitor the condition without treatment.
b. Steroid drops and order laboratory testing.
c. Steroid injection.
d. Anti-VEGF injection.
5. Which is the most likely etiology?
a. Roundworm.
b. Protozoan parasite.
c. Mycobacterium tuberculosis.
d. Bony mass.
For answers, see below.
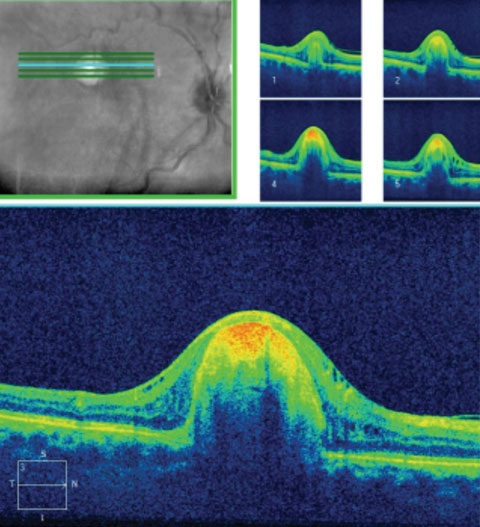 |
| Fig. 3. OCT 5-line raster of the lesion. How does this correlate to the fundus image? |
Diagnosis
This patient was seen in 2012 with no retinal abnormalities noted. At the 2016 visit, he presented with a yellowish-white, round, raised lesion with intraretinal fluid and macular edema in the right eye. No cells or flare were observed in the anterior chamber and vitreous was clear. SD-OCT of the macula confirmed intraretinal fluid. SD-OCT 5-line raster of the lesion showed a hyper-reflective mass with retinal pigment epithelium disruption. The differential diagnosis included toxocariasis, toxoplasmosis, tuberculosis, choroidal osteoma and sarcoidosis.Choroidal osteoma has a predilection for women and usually presents in the teenage years to the twenties. It presents as a minimally elevated bone-like mass of the choroid. We felt the clinical presentation, OCT findings and epidemiology were inconsistent with choroidal osteoma.
Active toxoplasmosis commonly presents with a significant amount of vitritis (“headlights in a fog”). There may also be spillover into the anterior chamber. The anterior chamber and vitreous were clear in our patient. It is possible that the lesion may now be inactive. Inactive toxoplasmosis is generally flat and has pigmentation at the edge of the chorioretinal scar. The lesion in our patient was elevated and there was no hyperpigmentation present.
Both sarcoidosis and ocular tuberculosis may present with a granulomatous anterior or posterior uveitis or both; however, sarcoidosis has a predilection in the African-American population. Our patient did not present with anterior or posterior segment inflammation. A complete blood work and chest x-ray were performed on the patient a few weeks prior to his presentation at the eye clinic and revealed no abnormalities.
Toxocariasis presents unilaterally as a posterior pole or peripheral granuloma. Fibrous bands may be present from the disc to the granuloma.1 Depending on the location, intraretinal edema, optic nerve edema and endophthalmitis can be noted.1 However, there are generally no chorioretinal scars adjacent to the granuloma, as is seen with toxoplasmosis scars.
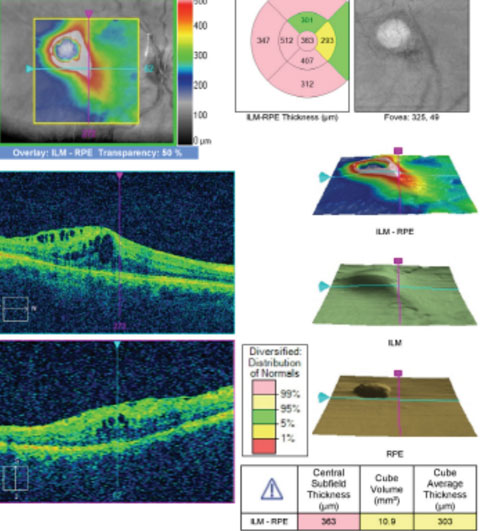 |
| Fig. 4. Macular cube OCT of the macula. What does it show? |
How the Worm Turns
As indicated, our patient had undergone a medical evaluation prior to his eye exam that included complete blood work, which was unremarkable, and a negative chest x-ray. Upon further questioning he confirmed that he obtained a dog three or four years prior to his exam, after which he noted poor vision in the right eye. Through a careful ocular history and clinical findings, including SD-OCT, we felt our patient had presumed ocular toxocariasis.Toxocariasis is an infection caused by a nematode—most commonly the roundworms Toxocara canis and Toxocara cati. Dogs and cats are carriers of the roundworm. It exists as visceral larva migrans and ocular larva migrans (OLM).2
Toxocara canis can be transmitted by ingesting contaminated soil (geophagia) or water. Children and young adults are commonly affected, but it can also be seen in adults. Larvae enter the human host and can travel to the liver, lungs, central nervous system and eyes.2 Ocular larvae enter the eye via choroidal, ciliary or retinal arteries where they are encapsulated in an eosinophilic granuloma due to inflammatory process.3
Aqueous and vitreous fluids may reveal increased eosinophils and toxocara antigens/antibodies. However, such tests are reserved for severe cases involving opaque vitreous and are usually deemed unnecessary for diagnostic and therapeutic reasons.1 Peripheral immunological tests such as the toxocara-specific ELISA are unreliable for detecting OLM. Ocular toxocariasis is primarily diagnosed on the basis of clinical criteria during an ophthalmologic examination.2
Treatment
Treatment for toxocariasis includes topical steroids for active inflammation, cycloplegic drops for ocular discomfort and even pars plana vitrectomy in the presence of significant inflammation or retinal detachment. Anthelmintics such as albendazole or thiabendazole is also used for active disease. Albendazole is the medication of choice due to its increased permeability to blood-brain barrier and lower toxicity than other antihelmetics.4Our patient was treated with Durezol (difluprednate, Alcon) QID and Nevanac (nepafenac, Alcon) QID OD to control the macular edema. Cataract surgery was recommended for the left eye post treatment of macular edema in the right eye. QuantiFERON gold and ACE testing were ordered to further rule out tuberculosis and sarcoidosis. Toxocara titers were also ordered.
Unfortunately, the patient was lost to follow-up and has not completed further testing. However, during a subsequent telephone conversation, he reported subjective improvement in vision in the right eye with the prescribed drops.
Dr. Patel is a resident at the VA Medical Center in Lexington, KY.
|
1. Tasman W, Jaeger E. Toxocariasis. In: The Wills Eye Hospital atlas of clinical ophthalmology. 2nd ed. Philadelphia, PA: Lippincott William & Wilkins;2001:297-8. 2. Despommier D. Toxocariasis: clinical aspects, epidemiology, medical ecology, and molecular aspects. Clinical Microbiology Reviews. 2003;16(2):265–72. 3. Yannuzzi L. Toxocariasis. In: The retinal atlas. Philadelphia: Saunders. 2010;369-70 4. Eberhardt O, Bialek R, Nagele T, Dichgans J. Eosinophilic meningomyelitis in toxocariasis: case report and review of the literature. Clin Neurol Neurosurg. 2005;107:432–8.1. |

