 |
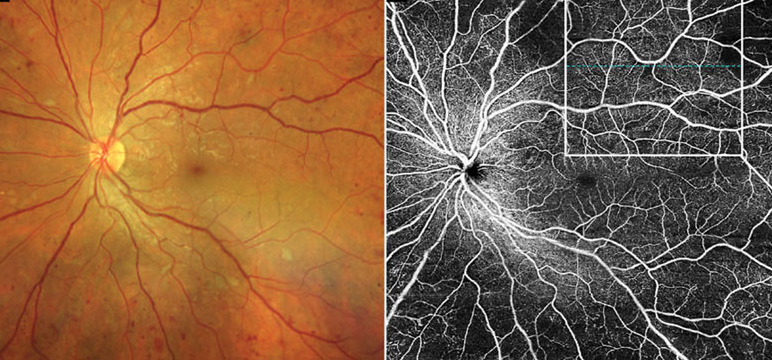
| Sex-based alterations appear to exist in diabetic microvascular disease, which should be considered in future clinical studies on DR and its OCT-A biomarkers. Photo: Carolyn Majcher, OD. Click image to enlarge. |
It’s known that men have a higher incidence, greater severity and faster progression of diabetic retinopathy (DR) than women. A recent study found that there are also observable differences in the microvasculature of men vs. women with diabetes on OCT angiography. The researchers urge that these sex-based alterations should be an important consideration in future clinical trials and studies on DR, as well as the implementation of OCT-A disease biomarkers.
To perform the study, the researchers obtained 3mmx3mm OCT-A macular scans of 1,809 patients with diabetes and 217 patients without diabetes. Of the patients with diabetes, 1,356 had no DR, 286 had non-proliferative DR, 126 had moderate NPDR, and 41 had severe NPDR or PDR. The following vascular parameters were recorded: (1) parafoveal vessel density, (2) vessel length density and flow index of the superficial capillary plexus (SCP) and DCP and (3) area and perimeter of the foveal avascular zone (FAZ).
The researchers made the following observations from the scans:
- Male sex was significantly associated with smaller FAZ area/perimeter and lower DCP vessel length density in patients with or without diabetes.
- Male sex in patients with diabetes was additionally associated with lower SCP vessel density/vessel length density and DCP vessel density.
- Being both male and diabetic conferred an increased reduction in DCP vessel density and vessel length density compared to sex-based changes in patients without diabetes.
- Larger FAZ perimeter, lower SCP vessel density and vessel length density, and lower DCP vessel length density were associated with worse visual acuity in those with diabetes.
In their paper on the study, the researchers summarized, “Our study highlights the importance of considering sex in future DR study designs whether from bench side or bedside, as diabetes may affect men and women differently. As more OCT-A data become available for normative DR databases and for disease prediction, sex needs to be considered as a potential confounding factor,” they concluded.
Zhang YS, Taha AT, Thompson IJB, et al. Association of male sex and microvascular alterations on optical coherence tomography angiography in diabetes. Transl Vis Sci Technol. 2023;12(11):30. |

